Spina Bifida

What is Spina Bifida?
Spina bifida is a condition where the spinal cord does not completely form in the first month of gestation. Every day about eight babies are born with a variation of spina bifida.
While it primarily affects the brain and spinal cord, it also impacts related body systems, such as the bowel, bladder, swallowing and skin to name a few. How these changes affect one child can vary greatly.
Scottish Rite treats neural tube defects, including:
- Myelomeningocele
- Meningocele
- Lipomeningocele
- Caudal regression
- Encephalocele
- Tethered cord
INTERDISCIPLINARY CARE FOR CHILDREN WITH SPINA BIFIDA
Spina Bifida Team
Our collaborative care team is dedicated to providing comprehensive care for your child’s optimal health and life.
Our Spina Bifida Program was established in 1992. For the past 30 years, our Spina Bifida clinic has continued to provide coordinated care to help each family and child navigate a successful life.
The Spina Bifida Program at Scottish Rite for Children provides a multidisciplinary team of experts from Developmental Pediatrics, Neurosurgery, Urology, Orthopedics, Physical and Occupation Therapy, Orthotists, and nurses, speech therapists and medical social workers to help treat each child’s individual needs.
Our Team
 Our Urology team works with each patient to identify goals and create treatment plans to meet their needs. Through management and care, our Urology team works to ensure that patients maintain normal renal function, transition through stages of urinary continence and achieve independence with personal care.
Our Urology team works with each patient to identify goals and create treatment plans to meet their needs. Through management and care, our Urology team works to ensure that patients maintain normal renal function, transition through stages of urinary continence and achieve independence with personal care.
96% of children with spina bifida have a neurogenic bladder. Our Urology teams help ensure each child’s bladder and kidneys are protected and strive to help each child achieve urinary continence. Most children with neurogenic bladders use intermittent catheterization to protect their kidneys and achieve continence.
The goal is to eliminate hostile bladder dynamics through medical management, reduce the need for surgery, maximize renal outcome, limit the effects of urinary tract infections and prevent antibiotic overuse, and establish a care routine that allows for urologic independence.
For children with spina bifida, we regularly perform a renal/bladder ultrasound, conduct urodynamic testing and measure serum creatinine to measure renal function.
Urinary Tract Infections (UTIs)
Nerves control many functions in our body. Spina bifida can damage the nerves that control the bladder and bowel. When this happens, your child needs help making sure the bladder empties regularly. If it doesn’t, bacteria can build up and cause an infection. A pediatric urologist can look at several different solutions to help prevent bladder and kidney problems in your child with spina bifida.
Urodynamics
Urodynamics is a pressure test of the bladder. “Uro” means urine, or related to the urinary system. “dynamics” means moving against pressure.
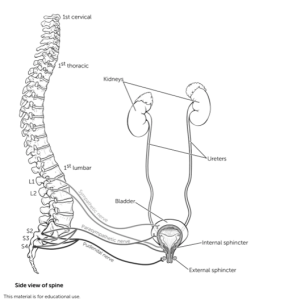
The lower urinary system comprises the ureters, bladder, urethra and sphincter muscle. The bladder is a balloon-like organ with a muscular wall that expands and contracts. Urine from your kidneys is stored in the bladder. The urine travels down tubes called ureters into your bladder. Urine is stored in the bladder until you decide to empty it. Emptying occurs by a contraction of the bladder muscle. A bladder contraction is similar to making a fist with your hand and squeezing it - the bladder contraction “squeezes” the bladder to empty the urine.
The sphincter [SFINK-ter] muscle sits right below the bladder. If you are not ready to empty your bladder, the sphincter muscle tightens like a knot at the bottom of a water-filled balloon. When you decide that it is time to empty your bladder, the sphincter muscle opens up, like untying the balloon.
Urination begins as the bladder pushes the urine out down a tube called the urethra. The urethra opens to the outside of your body, and urine is expelled. Urination takes place only when the muscles and nerves are working correctly. Messages are constantly being exchanged between the bladder and the brain through a pathway of nerves in the spinal cord. Sometimes, a head injury, stroke, or spina bifida will cause problems with a nerve pathway. Then, the bladder may not empty correctly. Persons sometimes have incontinence (leakage of urine) before or after having bladder or back surgeries. They need urodynamics testing to determine how well the nerves and muscles work.
The urodynamic test takes about one hour. Children may drink and eat a light breakfast or lunch before the test. If your child takes a bottle or pacifier, it is helpful to bring those with you. If your child takes medicine to help the bladder muscle (such as Ditropan®), this will need to be given two to three hours before the test. If your child has frequent problems with constipation, you should contact the nurse to receive bowel clean-out instructions. Children who have bladder control should not urinate for two to three hours before the test; they will be asked to empty their bladder into a special commode at the beginning of the test. This instruction does not apply to babies or children without bladder control.
One small tube, called a catheter, will be inserted into your child’s bladder. It will be used to fill the bladder with water and measure the movement of the bladder muscle as it fills and empties. A very small tube will be inserted into the rectum. It will measure the pressure put on the bladder when straining or coughing. Two patches or wires, similar to an EKG test, will be placed at the rectum or the opening of the urethra. These will monitor the sphincter muscle and its ability to hold urine in the bladder. Any discomfort felt during the test will go away within minutes following the test.
As the catheter fills the bladder with water through the catheter, the patient may be asked to describe what the bladder feels like. The patient may be asked to strain or cough several times. When the bladder is full, the patient will empty it. Some tests are performed using X-ray dye instead of water, and X-ray pictures will be taken throughout the test. The entire test will be recorded on a computer, and the patient can watch on a screen as it occurs. The health professional will explain everything as the test is being performed.
The catheters will be removed when the test is over. The patient may have a little discomfort where the catheters were placed. This should last only a few hours. A warm tub bath will help to ease any discomfort. Drinking an adequate amount of fluid (usually eight to ten glasses) is important (especially water) within 24 hours after the test. This will help prevent a urinary tract infection. An antibiotic medication may also be given before or after the test.
The patient may continue their diet, medications and activities as normal unless the doctor gives other instructions. After the test, the doctor will explain his or her findings and discuss treatment options.
Nielson-Ormeis, Betsy, “What is Urodynamics?”. Quality Care, Vol. 14, No. 3. pg.4, Summer 1996.
- Bruce Schlomer, M.D.
- Micah Jacobs, M.D.
- Yvonne Yuh-Ru Chan, M.D.
 Spina bifida is a word that encompasses a variety of neural tube defects. The area on the spinal cord and structural anomaly determines the surgical approach by our neurosurgery team.
Spina bifida is a word that encompasses a variety of neural tube defects. The area on the spinal cord and structural anomaly determines the surgical approach by our neurosurgery team.
Our Neurosurgery team helps manage the child’s shunts and other nervous system impairments, such as Chiari II malformation, spinal cord syrinx and tethered cords.
Hydrocephalus is a blockage of the flow of the cerebrospinal fluid (CSF), causing buildup of CSF in the ventricles. Hydrocephalus means the CSF that surrounds the brain is not draining fast enough. The CSF protects the brain and spinal cord, but if there is too much fluid, it can be dangerous. A shunt (tube) is inserted into the head to remove this fluid, draining to a part of the body where it can be removed naturally. If your child has a shunt, we recommend yearly follow-ups with a neurosurgeon. Contact the Spina Bifida Clinic nurse coordinator for help with follow-up appointments or questions.
A ventriculoperitoneal (VP) shunt is a tube with a valve that relieves pressure in the brain caused by hydrocephalus. It moves CSF away from the brain and into the abdomen.
Shunt Malfunction
80% of kids have ventricle enlargement that is treated with a VP shunt.
Below are common signs of hydrocephalus or shunt problems in patients with spina bifida.
If these symptoms occur, call your doctor or the Spina Bifida Clinic nurse coordinator.
| Infants | Toddlers | School-Age/Teens | Adults |
|---|---|---|---|
| Vomiting | Vomiting | Vomiting | Vomiting |
| Bulging fontanelle (soft spot) | Headaches | Headaches | Headaches |
| Lethargy (sleepiness) | Lethargy | Lethargy | Lethargy |
| Seizures | Seizures | Seizures | Seizures |
| Swelling or redness along the shunt tract | Swelling or redness along the shunt tract | Swelling or redness along the shunt tract | Swelling or redness along the shunt tract |
| Irritability | Irritability | Irritability | |
| Change in appetite | Decreased school performance |
Programmable Shunt
A programmable shunt is a specific type of shunt that can be adjusted from outside the body. These valves are designed to be adjusted by a strong magnetic field found in the external adjustment tool. Some of these valves may be susceptible to adjustment by strong environmental magnetic fields. Care must be taken to keep toys with magnets and other sources of magnetic fields away from the implanted device.
If your child has a programmable shunt and receives an MRI, a neurosurgeon must be present to check their setting after the procedure is complete.
The term “tethered cord” means the spinal cord can no longer move freely as the child bends and moves. All children with spina bifida are at risk for tethered cord. Some develop symptoms and problems with this.
Symptoms
- Loss or change in how the legs work
- Change in bowel or bladder pattern
- Back pain
- Unusual or severe pain in the legs and feet
- Scoliosis that gets worse very quickly
- Change in arch of feet or running in of ankles, curling of toes
These symptoms usually occur slowly over time and are progressive.
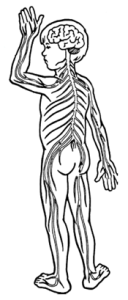
Cervical Nerves
The eight pairs of cervical nerves control movement and feeling in the shoulders, arms and hands.
Cranial Nerves (Brain Stem)
The 12 pairs of cranial nerves control movement feeling in the head, face, neck and arms.
Lumbar Nerves
The five pairs of lumbar nerves control movement of the hips, legs and feet.
Thoracic Nerves
The 12 pairs of thoracic nerves control movement and feeling in your chest.
Sacral Nerves
The six pairs of sacral nerves control the bladder, sexual organs and the colon. The first pair also helps control movement and feeling in the feet.
Alpha-fetoprotein (AFP)
AFP is a protein made by a developing fetus. The level of AFP may identify a possible neural tube defect.
Anencephaly
Anencephaly is a severe neural tube defect that occurs early in the development of an unborn baby. Anencephaly occurs when the upper portion of the neural tube fails to close. A large part of the brain and skull does not form. These babies do not survive.
Cerebrospinal fluid (CSF)
CSF is a clear liquid made in the brain that flows around the brain and spinal cord and then is reabsorbed.
Chiari II malformation
Chiari II malformation is a condition in which the cerebellum portion of the brain protrudes into the spinal canal. It is seen in most people with spina bifida.
Lipoma
Lipomas are benign, slow-growing tumors that come from fat cells. They are not cancer. A lipoma in the spinal canal can cause spinal cord compression.
Meninges
Meninges are membranes that cover the brain and spinal cord.
Meningocele
Meningocele is a form of spina bifida in which the covering of the spinal cord pushes through an opening in the spine, forming a fluid-filled sac. Typically, there is no nerve damage. Surgery is usually needed to remove the sac.
Myelomeningocele (MMC)
Myelomeningocele is from the Latin words for “spine” and “swelling.” This is usually referred to as spina bifida. A baby is born with a sac protruding from an opening in the spine. This sac contains nerves and part of the spinal cord.
Neural tube defect
The neural tube is a narrow channel that folds and closes between the third and fourth weeks of pregnancy to form the embryo’s brain and spinal cord. A neural tube defect occurs when the neural tube does not close. Examples of neural tube defects are anencephaly, MMC and meningocele.
Pseudocyst
A pseudocyst refers to a collection of fluid around the bottom opening of the VP shunt. It can create abdominal pain or cause the VP shunt not to work as well.
Syrinx
Syrinx refers to a fluid-filled pocket in the spinal cord. It can press on the spinal cord and cause damage.
- Brad Weprin, M.D.
- Dale Swift, M.D.
- Brett Whittemoore, M.D.
- Angela Price, M.D.
- Bruno Braga, M.D.
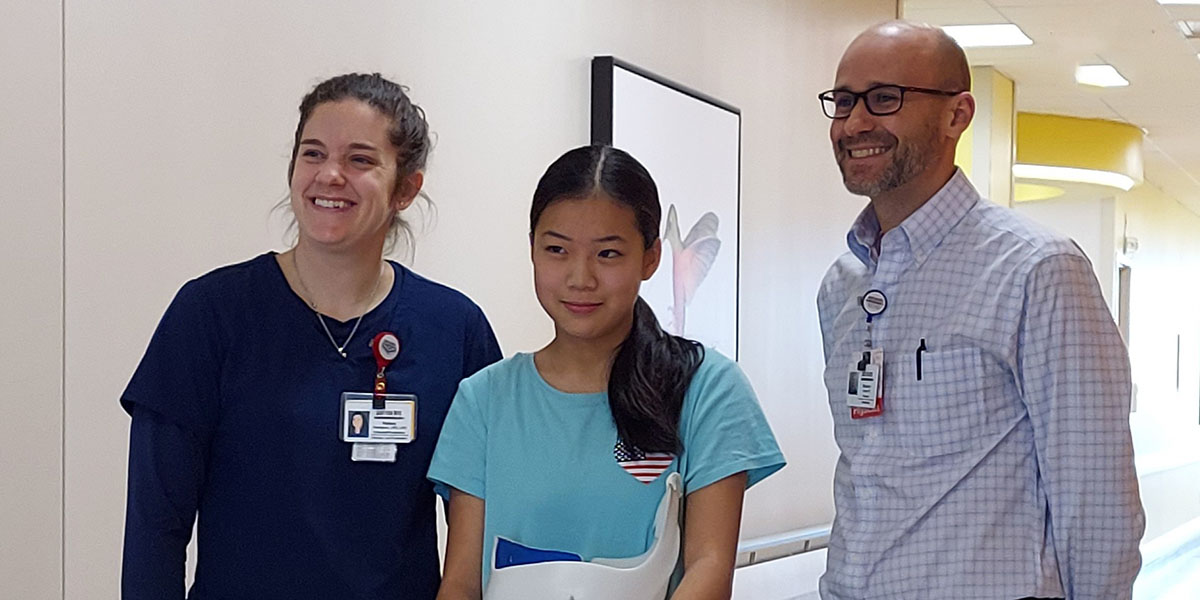
 Most children with spina bifida have orthopedic problems such as clubfoot, spinal curvatures and tightness of their knee, hips or feet. As children grow, it can become more physically demanding to walk. Our orthopedic team works alongside our orthotists and physical therapists to help determine what equipment or surgeries might be needed as the child grows.
Most children with spina bifida have orthopedic problems such as clubfoot, spinal curvatures and tightness of their knee, hips or feet. As children grow, it can become more physically demanding to walk. Our orthopedic team works alongside our orthotists and physical therapists to help determine what equipment or surgeries might be needed as the child grows.
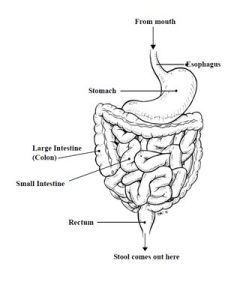 Children with spina bifida typically face nerve impairment to their bowel system. This can affect the motility and evacuation of stool. Our dietary team works with our nurse practitioners and doctors on individual bowel programs for each child.
Children with spina bifida typically face nerve impairment to their bowel system. This can affect the motility and evacuation of stool. Our dietary team works with our nurse practitioners and doctors on individual bowel programs for each child.
Young people with spina bifida may have problems with their bowels, but they can be managed. Every person is different. It will take time and patience to find the best program for your child. The program you use today may be different from the one used last month or last year. As your child grows and life changes, their bowel program may change, too. We are here to help you find the program that works for you and your child.
The Scottish Rite for Children staff (doctors, nurses, dietitians, therapists, pharmacists, psychologists and child life specialists) have developed an informational program for you and your child. The bowel program we use at Scottish Rite is like a set of building blocks. It begins with your child’s daily routines and habits and builds to include fluids, fiber, exercise, toileting and medication.
Bowel management continues throughout life. As your child gets older and things change, we will help you and your child make adjustments to the bowel program. The more consistent your child is with a bowel program, the more successful it is!
Maintaining good nutrition is an important aspect of any child’s health. A balanced diet will help assure that a child receives all the calories, protein, vitamins and minerals that he/she requires. In turn, this will promote growth and brain development.
The unique challenges associated with spina bifida mean nutrition plays a critical role in assuring each child develops appropriately and has an amazing quality of life. Because of this, a registered dietitian will meet with you regularly during your clinic visits. The dietitian will be able to educate you and your child from infancy to the late teen years on the role food, fluid and nutrients play in maintaining his/her health.
Fluids
Drinking adequate fluids is an essential part of feeling well. Water is essential to digestion in preventing constipation, promoting urinary health and delivering essential nutrients throughout the body.
- Add fruits, herbs or spices to water such as lemon, lime or apples and cinnamon.
- Use sugar-free flavoring liquids or packets.
- Carry and refill a water bottle throughout the day.
Fiber
What is fiber?
Fiber is the part of food that is not completely broken down by the digestive system, therefore it is not absorbed by the blood stream. Fiber stays in the intestines and acts like a “broom” to help move waste through the digestive system.
Types of fiber
Soluble Fiber
- Helps to slow down the movement of food through the digestive system, makes the “fullness” feeling last.
- When bowel movements are loose, soluble fiber soaks up the water to make stool firmer and slower to pass.
Insoluble Fiber
- Helps speed food through the digestive system.
- Insoluble fiber mixes with other waste materials in the intestines, adding bulk. This makes larger and softer bowel movements.
Most whole foods contain both types of fiber which help promote regular bowel movements. However, not enough fluid combined with a high-fiber diet can make constipation worse.
Ways to increase fiber
- Eat foods that are naturally higher in fiber: fruits, vegetables, grains, beans or nuts.
- Choose “whole grains” versus processed grain, for example, 100% whole wheat bread or brown rice.
- Ellen Dillard, R.D.
- Josiah Baker, R.D.
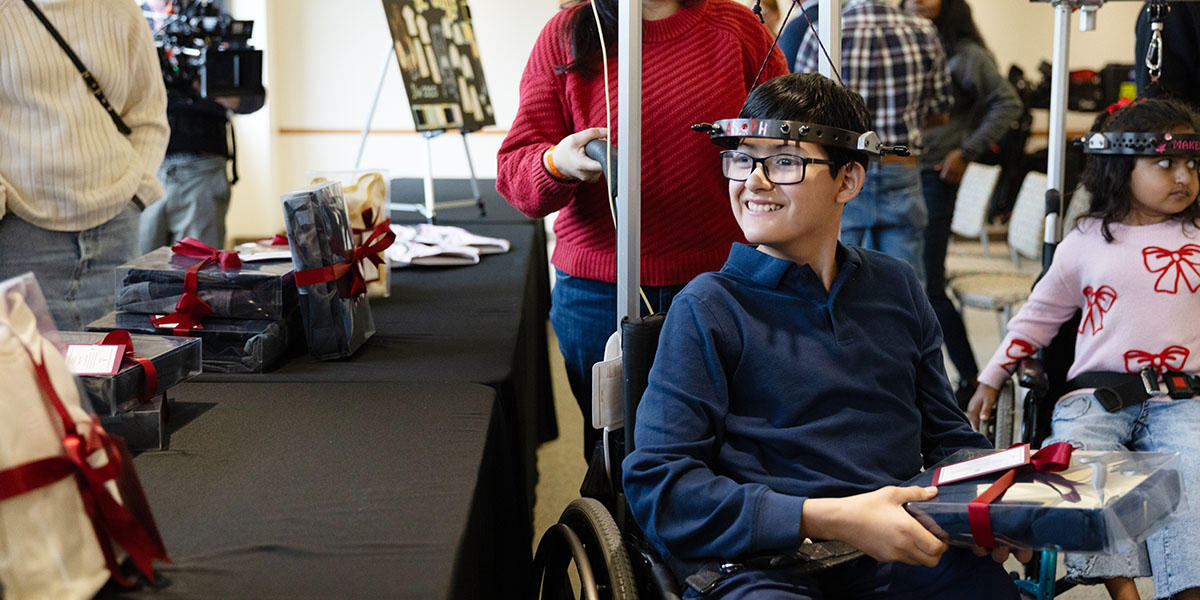
 Our Therapy Services team represents a cornerstone of our program. They evaluate each child’s developmental milestones and help set individual goals to achieve independence. They also assist with the specialized equipment that allows children to be as mobile as possible.
Our Therapy Services team represents a cornerstone of our program. They evaluate each child’s developmental milestones and help set individual goals to achieve independence. They also assist with the specialized equipment that allows children to be as mobile as possible.
Physical Therapy
Physical therapists are movement experts who improve the quality of life through hands-on care, patient education and exercise prescription. In the Spina Bifida clinic, our physical therapists will collaborate with patients, families, and the medical team to determine what interventions are necessary to maximize function and independence. Our physical therapists will provide consultative visits, evaluations and referrals for equipment and therapy needs. We also assist in identifying the need for referrals to additional medical providers.
Occupational Therapy
Occupational therapy (OT) focuses on maximizing a child’s independence in his or her everyday activities by facilitating the development of motor, cognitive, visual, social and adaptive skills. Our pediatric occupational therapists work with children and their families to help develop or regain function and/or techniques needed to participate in their activities of daily living (ADLs), which may include dressing, bathing, eating, grooming, play, school or work tasks. Our OTs at Scottish Rite serve our children with spina bifida in three different settings: clinic, inpatient and outpatient.
Our OTs can perform catheterization screenings to assess appropriate underlying skills needed for self-catheterization, help coordinate equipment concerns if not able to ameliorate in clinic and check-in periodically for any needs. Should your child need any ongoing services, our OTs can either refer to outpatient services at Scottish Rite for Children or another appropriate provider depending on needs presented.
Therapeutic Recreation
Therapeutic recreational specialists work with children and their families to assess an individual’s interests and abilities and then match those to the resources available in their community. Recreational activities not only encourage fitness and wellbeing, but also improve self-esteem.
The undeveloped or damaged nerves cause differences in the sensation or feeling in an individual's skin. This often leads to wounds and pressure sores.
What is a Pressure Ulcer?
A pressure ulcer is an injury to the skin that can occur when a person stays in one position too long. The skin pressed against a hard surface can become a sore because the blood flow to the area decreases or stops. This causes the skin to die, resulting in the pressure ulcer. A pressure ulcer starts on the inside of the body and works its way to the skin’s surface. It may take up to seven days after the skin is injured for the pressure ulcer to appear. A pressure ulcer can be a reddened area of skin or it can be an open area that starts at the bone and breaks through the skin.
Pressure ulcers occur when there is constant pressure on the skin, especially over bony areas such as the tailbone, hip, spine, knee, ankle, heel, shoulder blade or back of the head. The skin gets squeezed between the bony area and something hard (like a mattress, chair, brace, cast, swimming pool ledge or foot plate of wheelchair). Skin breakdown can also happen in skin folds.
Risks
- The skin can get injured from shear, friction, pressure, moisture and heat.
- Shear — tissue rubbing against tissue, causes deep wounds
- Friction — rubbing a body part against a surface
- Pressure — skin pressed between bone and a hard surface Heat exposure — sunburn, hot water, hot cement etc.
- Moisture— increases shear/friction effects (urine, stool, sweat, and wound drainage)
What are the risk factors for pressure ulcers or skin problems?
- Body parts with little or no feeling—usually buttocks, legs and/or feet
- Movement — using a wheelchair, “bunny hopping” or commando crawling
- Incontinence — urine and bowel movements can cause skin irritation
- Use of braces — especially in the first month or after six or seven months of wear
- Being underweight or overweight
- Summer — more wounds occur during this time due to outdoor activities or heat
Prevention
- Check the skin each morning and each evening for red or open areas. Teach your child to use a skin inspection mirror to view hard-to-see areas.
- Use backpacks and cup holders on wheelchairs—do not use the wheelchair seat as a storage area.
- Check the wheelchair cushion each day to make sure it’s in good working order. Contact the wheelchair vendor or therapist if the cushion needs to be repaired.
- Remind your child to do weight shifts every 15 minutes with all activities—while in the wheelchair, biking, horseback riding, etc.
- Use custom gel pads over bicycle seats and horse saddles to reduce pressure to the buttocks.
- Prevent burns by using sunscreen when outdoors. Hot sand, hot concrete, hot wood, hot plates or hot metal can burn skin, too.
- Know where your child’s feeling starts and stops.
- Leave wheelchairs in shady areas when not in use to prevent burns from skin contact with the metal parts of the chair. Feel the wheelchair cushion for hot areas.
- Wear swim shoes for all pool activities to prevent scrapes on the feet.
- Check the braces often to see if adjustments need to be made for growth.
- Use barrier cream for bowel cleanouts and for incontinent episodes. Keep your child on a bowel program.
- Wear shoes and socks always! Use long pants for crawling.
- Do extra skin checks after periods of high activity.
- Keep your child at a healthy weight.
- Talk with medical or nursing staff about your child’s wound risk factors prior to any surgery.
- Share these ideas with teachers and school nurses so care can be taken.
The research program in Spina Bifida department aims to collaborate with clinicians and other departments to collect clinical data and to enhance the care to infants, children, youth, and adults with spina bifida and their families. Learn more about our current research studies.
National Spina Bifida Registry
The Spina Bifida Association's Professional Advisory Council set up the National Spina Bifida Patient Registry through the CDC. It is used to help collect scientific data needed to evaluate existing spina bifida patients. The data produces information from patients to better under the associations between medical care and health outcomes. Spina Bifida patients at Scottish Rite are invited to participate but are not required.
Previous Works
I. Longitudinal Patterns of Latex Allergy Among a Large Populations of Individuals with Spina Bifida
II. Psychotropic Medication use in Children and Youth with Spina Bifida
Publications
"Education and Employment as Young Adults Living with Spina Bifida - Transition to Adulthood: The National Spina Bifida Patient Registry". Developmental Medicine & Child Neurology. 2022.
6-Minute Walk Test in Ambulatory Children with Spina Bifida
Many children with spina bifida are able to walk less as they get older. The six-minute walk test is a helpful assessment that can determine a patient’s functional exercise capacity. This study aims to establish reference values in patients with spina bifida. In the future, we will look at the distance that a patient walks in a six-minute time frame and can compare their score to these reference values. This will help us identify differences in exercise capacity between patients.
Previous Works
I. Longitudinal Patterns of Latex Allergy Among a Large Populations of Individuals with Spina Bifida
II. Psychotropic Medication use in Children and Youth with Spina Bifida
 As children grow to adulthood, there are many bridges to be crossed:
As children grow to adulthood, there are many bridges to be crossed:
- From infancy to toddlerhood, and from young child to teenager
- From preschool to high school, to job training or college and beyond
- From living at home, to becoming a member of the community
The goal of transition at Scottish Rite is the gradual developmental of self-directed care responsibilities from the adult to the young adult.
Through this process, your Spina Bifida team at Scottish Rite plans to give optimal support to the youth/young adult and the family. This will be based on individual need within the context of the medical health system, community, and further education or workforce or other activities appropriate to the individual.
This process will involve multiple steps, and that is why it is important to address transition at every clinic visit. Formal planning for transition in the program begins at about age 14 – or sooner if the situation demands.
It will be important to set aside time with our social worker during your annual visits. Our social worker is our key resource to helping families navigate resources including legal needs, referrals, insurance and medical providers.
Transition is a process. Our goal is to successfully bridge the gap between pediatric and adult health care and ensure that your family is well supported while crossing that bridge.
Resources
Health History Interactive Form (English | Spanish)
Setting up a Medical ID on a iPhone (English | Spanish)
Setting up a Medical ID on a Andriod (English | Spanish)
Care Coordnation for Young Adults (English | Spanish)
TRAQ5 (English)
Guidelines for the Care of People with Spina Bifida (English)
Clinical Care Partner
The Spina Bifida Association (SBA) Clinic Care Partner program is an initiative that works to identify the needs of people with Spina Bifida as well as identify clinics with the best outcomes. Clinics who become SBA Clinic Care Partners implement best practices so that people with Spina Bifida receive the best care possible in order to have fulfilling lives. Check out the Guidelines for the Care of People with Spina Bifida.
Scottish Rite for Children is recognized as a SBA Clinic Care Partner.

Our Experts
Michelle Maldonado, CPNP

Megan E. Johnson, M.D.
Karl E. Rathjen, M.D.

Christine Murphy, M.D.
Cherlyn Caneda, CPNP, RNFA

Emily Chapman, CPNP-PC
Latest news: Spina Bifida
D CEO: Scottish Rite and TWU Team Up for Adaptive Fashion
At Texas Woman’s University, a fashion design class took learning beyond the classroom by focusing on how their skills could help the community. The course partnered with Scottish Rite for Children after…
How Danielle Unlocked Her Passion Through Scoliosis Treatment
Sixteen-year-old Danielle is an innovator at heart. During her scoliosis treatment, she discovered solace in the hum of motors at her school’s robotics club. “Robotics helped me power through my treatment,” Danielle…
D CEO: 2025 Excellence in Healthcare Award Winners Announced
D CEO revealed its 2025 Excellence in Healthcare Award winners. The program recognizes outstanding healthcare executives, practitioners, organizations and other innovative industry leaders in the Dallas region. Attracting more than 100 nominations, D…
CBS11: BMW Dallas Marathon Spotlights Children’s Resilience
As runners prepare for the BMW Dallas Marathon, organizers highlight that not all victories happen on the course. Proceeds benefit Scottish Rite for Children, which is spotlighting young patients whose resilience inspires…
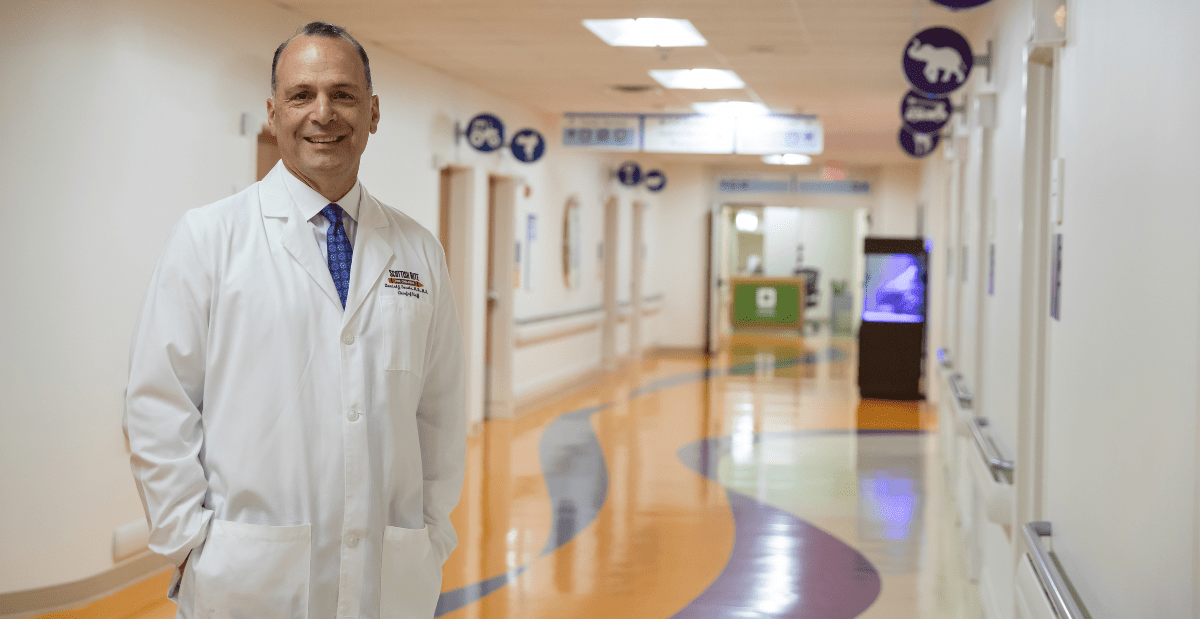
Becker’s: Leading Pediatric Orthopedics at Scottish Rite with Dr. Daniel Sucato
Chief of Staff Daniel J. Sucato, M.D., M.S., speaks with Scott Becker on the Becker\'s Hospital Review Podcast about Scottish Rite for Children, ranked No. 1 in the nation for pediatric orthopedics…
CBS11: North Texas Teen Overcomes Spinal Surgery to Run in BMW Dallas Marathon
Seventeen-year-old Riley is preparing for the BMW Dallas Marathon, an achievement she once thought impossible. Diagnosed with scoliosis in seventh grade, Riley endured worsening pain until spinal surgery at Scottish Rite for…
Scottish Rite for Children Wins Award for Reducing Opioid Use Following Scoliosis Surgeries
Scottish Rite for Children has received one of Texas’ highest honors in health care quality — the Texas Hospital Association’s (THA) Bill Aston Award for Quality — for its innovative program that…
Inside DFW: How Art Helped Lorena Heal
Now in its fourteenth year, Summer Colors showcases original artwork from both established and emerging artists, including Lorena, a young patient at Scottish Rite whose journey through treatment inspired her to give…
CBS Texas: Livvy and Georgia go from patients to performers
During their time at Scottish Rite for Children, 12-year-old Livvy and 13-year-old Georgia found inspiration from the doctors, nurses and fellow patients who supported them through scoliosis. \"This place will always have…
CBS19: High School Graduate Dreams of Radiology Career After Her Care at Scottish Rite for Children
18-year-old Fernanda was diagnosed with scoliosis in sixth grade. \"It was difficult, but I just had to keep going through it,\" Fernanda says. Her experience at Scottish Rite for Children transformed from…