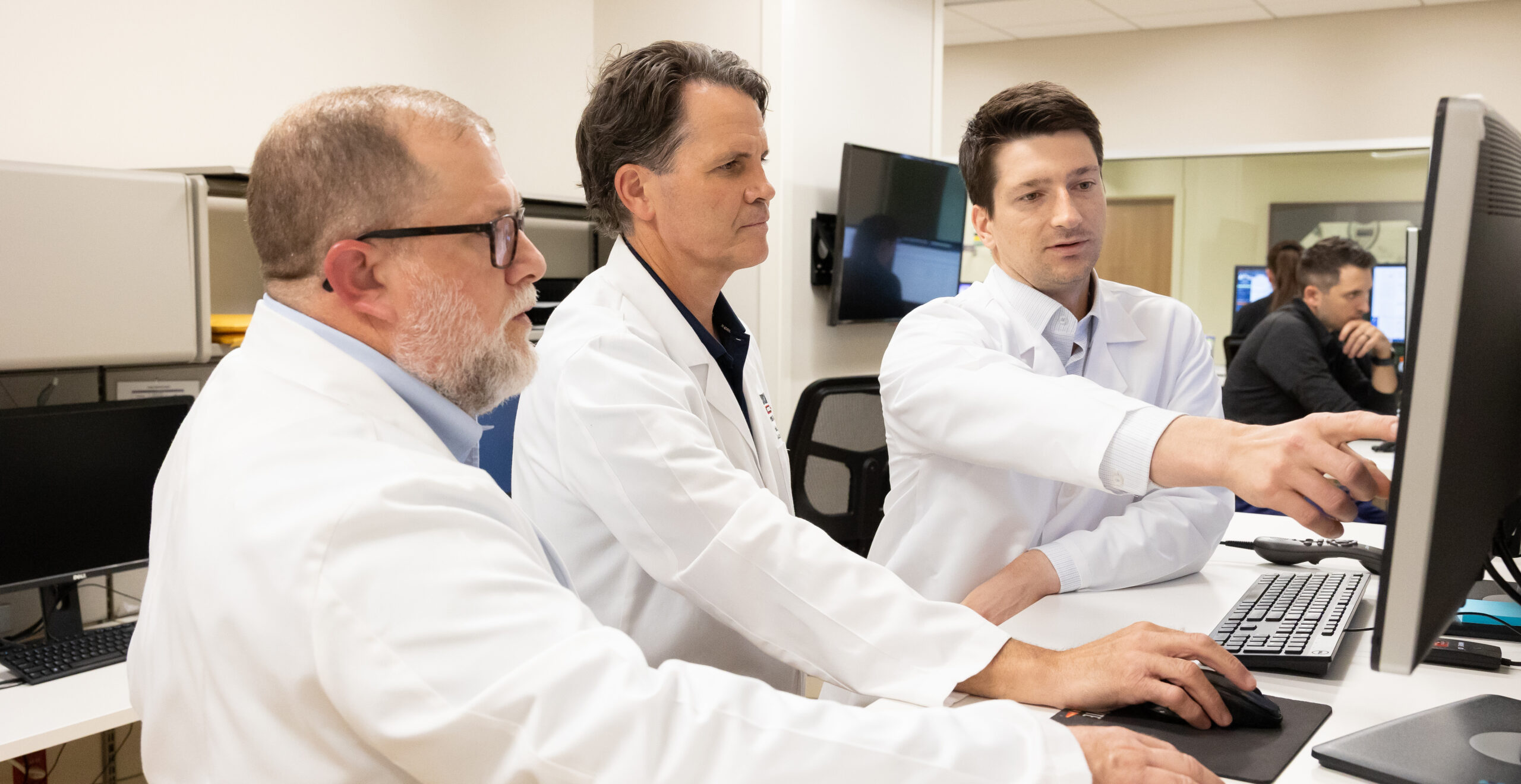
Last year, biomechanical researchers at Scottish Rite for Children began providing high school teams with resources typically only available or affordable at the professional and collegiate levels. They created pre-season injury-prevention trainings, tailored for...