A large, active growth plate is positioned near the ball of the shoulder joint in skeletally immature athletes.
The extreme rotation of the arm in the cocking phase of throwing is relatively unrestricted. The shoulder is pushed to its limits with every pitch. Over time, the growth plate may be stressed by this repeated rotation. This may lead to stress in the growth plate that results in widening of the growth plate and a bruising bone pain around this area.
Training focused on form, not force, is critical for young athletes in overhead and throwing sports. This includes following for pitch count guidelines and progressing to advanced pitches at appropriate ages. Periods of rest are important to allow the tissues to recover between events and seasons. Stabilization exercises for the shoulder blade can improve posture and therefore form. Since pitching requires control and strength in the entire body, hip and trunk strengthening is an important component of training.
Early signs and symptoms of Little League Shoulder include pain in the shoulder after throwing that resolves with rest. Pain that doesn’t resolve after rest may be an indication of a more advanced problem needing further evaluation.
A thorough history for an athlete includes a conversation about past medical history, the injury or onset of symptoms, as well as sport exposure. Sport exposure includes what position, frequency of practices and games, length of seasons, and number of pitches, for baseball. X-ray imaging of the injured shoulder and opposite side may be ordered to help to rule out a fracture and to evaluate the growth plate for signs of stress.
With early recognition, forced rest can lead to a successful return to sport with no permanent changes in the bony structure. With ongoing symptoms and continued throwing, changes to the bony structure or soft tissues may result in permanent changes in shoulder mobility. Symptom management with anti-inflammatories and ice may be required, but often, resting the arm provides relief.
After a period of forced rest, often 6-8 weeks or longer, the pain will typically improve and the athlete may return to throwing in a progressive routine: throwing short sessions and slow pitches and progressing to longer sessions and faster pitches. Rest is recommended for any symptoms that return with throwing.
Successful pitching requires the arm to tolerate large forces. The tissues in the front of the shoulder become longer with the repeated stretching at the high speeds. Over time, the tissues in the back become short and together, this limits the range of motion of the shoulder.
It is unclear if this change in shoulder motion is necessary for successful pitching. Therefore, preventing symptoms related to this change is the goal. Recognizing signs and symptoms and responding promptly with proper rest are the most important steps.
Generalized pain in the front of the shoulder may be a sign of changes in the shoulder, or it may be the sign of an injury.
A thorough history for an athlete includes a conversation about past medical history, the injury or onset of symptoms, as well sport exposure. Sport exposure includes what position, frequency of practices and games, length of seasons, and number of pitches, for baseball. Imaging will be ordered when the physical exam suggests other tissues may have been damaged.
Treating the change in motion may not be necessary, unless the symptoms are directly related to the changes in motion. Treatment is typically recommended so that the athlete can learn exercises to reduce his risk of injury because of the excessive rotation in one direction. This would include shoulder blade stabilizing exercises, among other exercises.
Returning to sports is dependent upon the athlete’s ability to pitch with proper form and to be symptom free. Other diagnoses and treatment plans may delay the athlete from returning to sports.
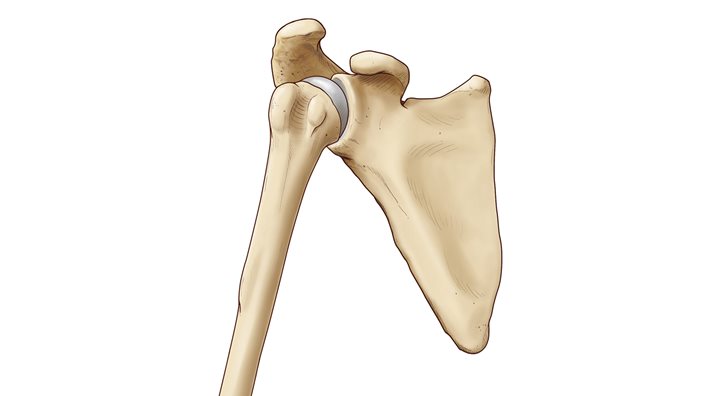
The mobility of the shoulder joint allows for extreme motions in sports like baseball, gymnastics and volleyball, but that also puts the shoulder at risk of injury. The socket, called the glenoid, is a shallow cup, and the ball of the upper arm bone, the humerus, can feel unstable or even slip out of the socket completely. Some athletes are predisposed to this because of naturally weak ligaments or changes to the bony surfaces with repetitive activity.
Extreme forces on the shoulder when the shoulder is in certain positions can result in the ball moving out of the socket completely. Approximately 9 out of 10 athletes that have experienced a shoulder dislocation are likely to experience another.
Strengthening exercises for the shoulder’s rotator cuff muscles and muscles around the shoulder blade can improve stability. These exercises can also improve the body’s ability to respond to changes in movement. This is a combination of proprioception and neuromuscular control.
Severe pain with a traumatic dislocation often improves quickly when the shoulder is returned to its normal position. With repetitive dislocations, there may be no pain because the tissues have changed over time to allow this movement to occur easily.
A thorough conversation about episodes of instability and dislocation will help a provider confirm the diagnosis. X-ray or other imaging of the shoulder may be ordered to help to rule out a fracture and to evaluate the joint surfaces and soft tissue for changes.
With early recognition, physical therapy can help to improve pain, motion and stability. Most athletes return to play after an initial event. In cases of repetitive events, surgical reconstruction may be required. Physical therapy after a reconstruction will help to regain shoulder mobility and strength.
In non-operative treatment plans, sports participation may only be limited for a short period of time to allow focused rehabilitation. After a surgical procedure, restrictions from sports and other activities will vary from 4-6 months, and returning to sports will be most safe after completing a rehabilitation program designed specifically for the athlete.
The bony surface of the socket is very shallow. A circle of soft tissue, called the labrum, sits on the edges to make the socket deeper. As the ball moves around in the socket, the labrum may become stretched or compressed by the bone or the other soft tissues attached.
A labral tear can occur in a single traumatic event like a dislocation. In adults, this is more likely to occur with repetitive movements that cause wear on the tissue and ultimately, allow a tear. Athletes that are softball pitchers, volleyball players and baseball pitchers are more likely to have overuse injuries to the labrum. Repetitive episodes of shoulder instability, such as a dislocation, can lead to a labral tear.
Stabilization exercises for the shoulder and shoulder blade can improve the strength of the muscles. More importantly, the stabilization exercises can put the shoulder in its best position, both for performance and for injury prevention.
Pain with activity, especially throwing and overhead activity. Pain and instability are common with labral tears. Range of motion is usually normal.
A thorough conversation about symptoms, activities and any injuries can help a provider make a preliminary diagnosis. Radiographic X-rays and an MRI may be ordered to assess the bone and soft tissue, including the labrum. There are names for damage to different areas of the labrum. SLAP or Bankhart lesions are the most common tears in adolescent athletes.
Not all labral tears will require surgery. The athlete’s symptoms, like pain and instability, and ability to perform daily activities, will help to determine if surgical treatment is required.
In non-operative treatment plans, sports participation may only be limited for a short period of time to allow focused rehabilitation. After a surgical procedure, restrictions from sports and other activities will vary from four to six months, and returning to sports will be most safe after completing a rehabilitation program designed specifically for the athlete.
The collarbone is attached to the shoulder with soft tissues, including tough ligaments.
With an injury like a strong blow directly on the shoulder from a hit or a fall, or a fall on an outstretched arm, the ligaments holding the collarbone can tear. In some cases, the collarbone visibly separates from the shoulder at the acromioclavicular (AC) joint.
Proper equipment for the position played and proper tackling form for the tackler and the player being tackled can reduce the risk of an AC joint separation.
Typically, there is severe pain and limited ability to move the shoulder at the time of injury. Swelling and bruising follow soon after.
The joint may appear abnormal in a visual exam. With a physical exam, there is tenderness at the AC joint. An x-ray is typically ordered to rule out a clavicle or collarbone fracture. An AC joint separation is categorized based on the severity of the injury.
In the early phase, rest and activity restrictions are recommended. Immobilization in a sling helps to rest the shoulder during healing. Most cases will heal on their own with these treatments and surgery is rarely needed.
Follow-up physical exams are important to assess the tightness of the healing ligament and the mobility of the shoulder. Returning to sports before healing puts the shoulder at risk of a more severe injury.
The mobility of the shoulder joint allows for extreme motions in sports. A complex network of nerves, called the brachial plexus, extend from the neck into the arm to allow the hand to feel and move.
An extreme stretch to the brachial plexus can cause short-lasting symptoms with damage to the nerve tissues. Most often, this injury occurs with a fall on the head and shoulder. This is a common injury in high school and collegiate football players and occurs less frequently in adolescent athletes.
Proper equipment for the position played and proper tackling form for the tackler and the player being tackled and reduce the risk of a burner.
Neurological symptoms include numbness, tingling and pain in the arm, only on one side. These typically last less than 15 minutes, but in some cases, may last days or weeks. Because the injuries can occur together, the athlete should be evaluated for signs and symptoms of a sports concussion.
The mechanism of the fall, combined with the description of one-sided neurological symptoms, is typically sufficient for a diagnosis. Imaging may be recommended to rule out other problems in the neck and for patients with persistent symptoms or a history of multiple stingers.
In the early phase, rest, a sling for comfort and NSAIDS may be used. Typically, healthy athletes will recover quickly and will not need treatment. Surgical treatment for this is extremely rare. Rehabilitation may be recommended for neck and shoulder strengthening.
Without signs and symptoms of another injury, athletes can typically return to sports quickly when they are symptom free.
The collarbone is the only bony attachment of the shoulder to the trunk. Soft tissues surround the collarbone to provide stability and also a great amount of mobility for the arm.
A collarbone fracture most often occurs with high force traumatic events.
In some sports, like football, pads and gear may protect the collarbone. In other sports, proper balance of strength and flexibility of the neck and shoulder muscles may aide in preventing collarbone injuries. These injuries are often unpredictable, and likely unpreventable.
Pain at the site of the break is the most typical symptom with this injury. In some cases, damage to other vessels and nerves in this area may cause symptoms further down the arm. An athlete with a collarbone fracture naturally places the arm in a guarded position by wrapping the forearm across the stomach. The shoulder, on the injured side, often appears to be lower than the non-injured side.
X-rays are most useful in confirming the diagnosis and to guide treatment planning.
Non-operative approaches include using a sling to immobilize the arm for comfort, and monitoring the natural healing process of the bone. This has been shown to be effective in most cases. Surgical intervention is considered where natural healing is not likely to promote normal function of the shoulder.
After a period of 6-8 weeks, with pain resolved and x-ray evidence of good bone healing, an athlete is often returned to sports with instructions to progress as tolerated. For some collision sports like hockey and football, a longer healing time may be recommended.





.jpg?width=1200&height=619&ext=.jpg)