Sports Medicine

WHAT IS SPORTS MEDICINE?
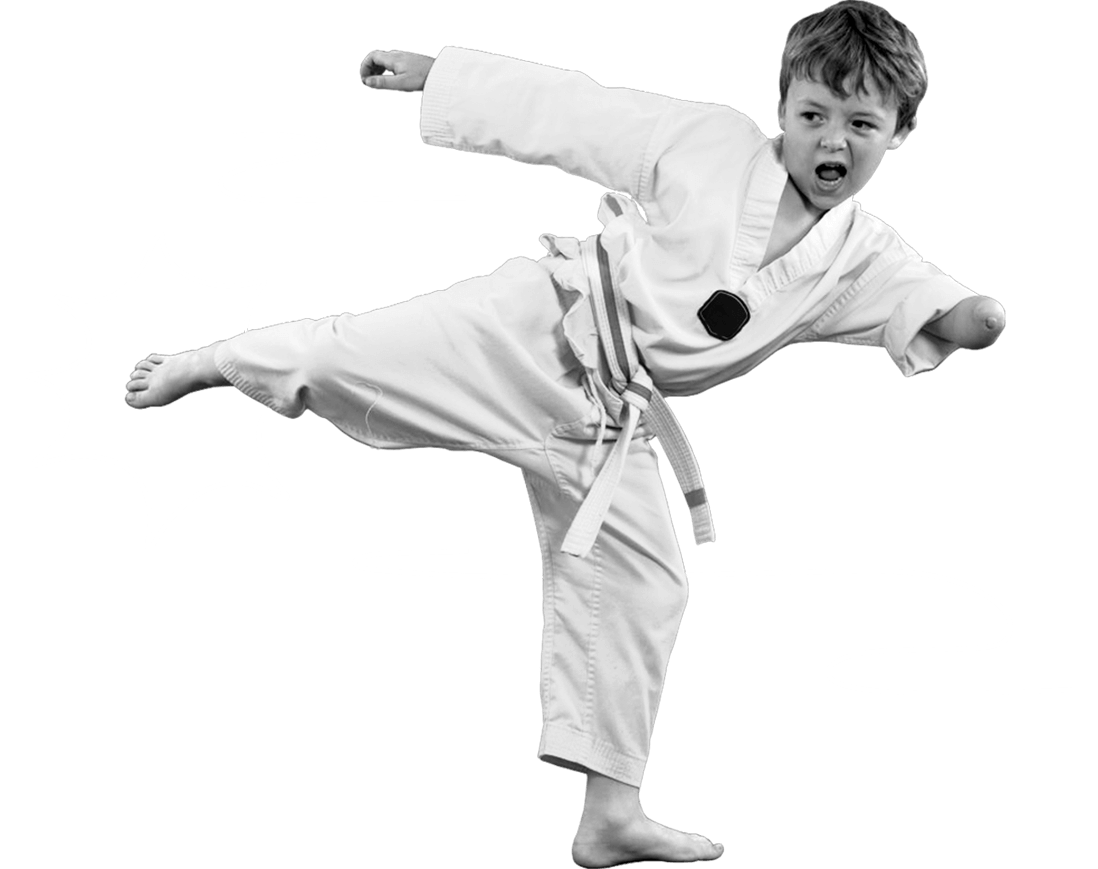
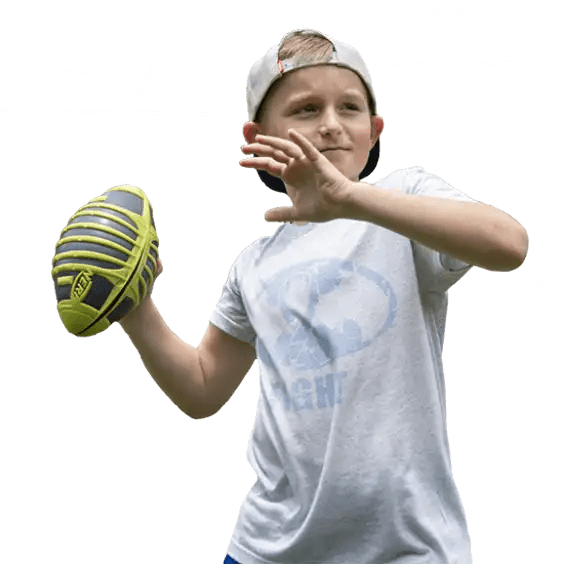
Sports medicine is a medical and surgical specialty that considers the comprehensive needs of athletes and provides management for sport-related injuries and conditions. Young and growing athletes are highly competitive and have unique conditions that require care by a pediatric team of experts.
Our world-renowned sports medicine experts are ready to help your injured athlete get back in the game. We have unparalleled experience providing non-operative and arthroscopic care to treat common sport-related injuries including concussions, ligament injuries and cartilage conditions in the knee, ankle, shoulder, elbow and hip in young and growing athletes.
Board-certified pediatricians, pediatric orthopedic surgeons, physical therapists, athletic trainers, psychologists and other sports medicine specialists work side by side with each athlete, their parents and coaches to develop the best game plan for treatment, rehabilitation and safe return to sport.
We love celebrating the achievements of our current and former athletes. Whether you’re overcoming an injury or reaching new heights in your sport, we want to hear your story. Share Your Story with us.
Sign up to receive our digital newsletter with tips and insights for parents of young athletes.
AREAS OF TREATMENT
Ankle
 Young athletes are more likely to break a bone than to have an ankle sprain. Unlike fractures, subtle injuries to the bone or the soft tissue covering the bones may be difficult to diagnose. Symptoms that don’t get better with rest may need a thorough evaluation by a pediatric specialist. Recognizing and responding to symptoms of ankle instability or pain with repetitive activity can help keep young athletes on the field. The risk of ankle injury can be reduced with good training, proper shoes and field maintenance.
Young athletes are more likely to break a bone than to have an ankle sprain. Unlike fractures, subtle injuries to the bone or the soft tissue covering the bones may be difficult to diagnose. Symptoms that don’t get better with rest may need a thorough evaluation by a pediatric specialist. Recognizing and responding to symptoms of ankle instability or pain with repetitive activity can help keep young athletes on the field. The risk of ankle injury can be reduced with good training, proper shoes and field maintenance.
Conditions we treat:
- Ankle instability
- Ankle sprain
- Ankle fractures
- Stress fractures of the foot and ankle
- Cartilage conditions such as osteochondritis dissecans (OCD)
- Sever’s disease
Elbow
 The elbow is a combination hinge-and-pivot joint made up of three bones: the upper arm bone (humerus) and the two bones in the forearm (radius and ulna). The hinge part of the joint lets the arm bend like the hinge of a door; the pivot part lets the lower arm twist and rotate.
The elbow is a combination hinge-and-pivot joint made up of three bones: the upper arm bone (humerus) and the two bones in the forearm (radius and ulna). The hinge part of the joint lets the arm bend like the hinge of a door; the pivot part lets the lower arm twist and rotate.
Muscles, ligaments and tendons hold the elbow joint together.
Cartilage, or soft tissue, protects the bony surfaces. It’s also found in young bones at areas that are still growing. These growth areas are at risk for injury.
Elbow injuries in young athletes are on the rise, partly due to year-round training and competition. Overuse injuries often occur in throwing sports and gymnastics. Early recognition of signs and symptoms can prevent problems and even career-changing injuries. In youth sports, preventing elbow injuries, particularly those requiring surgery, is a priority.
This is the most common condition in child athletes, typically caused by excessive throwing. The throwing motion puts stress on the middle side of the elbow because the tendons and ligaments of the forearm are pulling on the growing bone.
Pain typically occurs on the inside “bump” of the elbow during or after activity like throwing or pitching. Repeated pulling can tear ligaments and tendons away from the bone. This tearing may pull tiny bone fragments with it in the same way a plant takes soil with it when uprooted. This can disrupt normal bone growth, resulting in deformity and instability with throwing.
SYMPTOMS
- Elbow pain with throwing or after activity
- Pain and tenderness on the inside of the elbow (on the bump)
- Soreness for days to weeks
- Worsening control with throwing
- Inability to throw desired distance
- Difficulty fully straightening or bending the elbow
- Locking of the elbow
TREATMENT
- Rest. Continuing to throw may lead to major complications and jeopardize a child’s ability to remain active in a throwing sport.
- Common recommendations include 2-4 weeks of complete rest.
- Apply ice packs to bring down any swelling.
- Proper stretching and strengthening.
- May require a cast or splint if the pain does not resolve with rest.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Focused training to improve throwing form is needed.
- Surgery to stabilize the medial epicondyle is rarely necessary, especially in girls over 12 years and boys over 14 years.
An avulsion fracture occurs when the muscles and tendons pull off a piece of bone that is connected by cartilage to the main bone. A strong pull of the forearm muscles, during a pitch, for example, can cause an avulsion fracture of the medial epicondyle on the inside of the elbow.
With this injury, the athlete will typically hear a pop and will have severe pain, swelling and bruising. The child may or may not have had elbow pain before the injury. With operative or nonoperative treatment, most kids may return to the same level of sports following treatment.
SYMPTOMS
- May hear a pop or giving way
- Immediate pain on inside of the throwing elbow
- Immediate, visible swelling and bruising
- May have pain with wrist movement
- May have numbness or tingling in the ring finger and little finger
- Unable to bend the elbow or pick up heavy objects
TREATMENT
- Ice may be helpful to reduce inflammation in early stages.
- Anti-inflammatory medication may be needed.
- For fractures in good position, a splint is recommended for 2-3 weeks.
- In all cases, aggressive range of motion early in healing stages (within 2-3 weeks) is recommended.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Strengthening and proper throwing progression 8-12 weeks following injury.
- Focused training to improve throwing form is needed.
With repeated throwing, inflammation of the cartilage on the back of the elbow can occur. When this occurs, a growing athlete may have pain during follow-through or when straightening the elbow. In the older adolescent, bone spurs and stress fractures can also occur in this area. Without proper rest and treatment, pieces of cartilage can tear away; removal of these loose pieces may require surgery.
SYMPTOMS
- Pain in the back of the elbow during follow-through and when straightening arm
- Pain in the back of the elbow that becomes gradually worse over time
- Inability to completely straighten the arm
- Popping and locking may be present, but is rare
TREATMENT
- Rest. Continuing to throw with this problem may lead to major complications and permanently jeopardize a child’s ability to play.
- Common recommendations include 2-4 weeks of complete rest.
- Ice pack may help reduce inflammation.
- Anti-inflammatory medication may be needed.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Focused training to improve throwing form is often necessary.
- Surgery is only needed in severe cases.
Excessive throwing may also lead to a less common condition called osteochondritis dissecans (OCD). Pulling of the muscles on the inside of the elbow causes pushing, or compression, of the bones on the outside. The pressure on the immature bones can loosen a piece of the bone and cartilage.
SYMPTOMS
- Dull achiness on the outside of the elbow
- Pain that worsens with activity and improves with rest
- Pain that gradually worsens over time
- Inability to completely straighten the arm
- Popping and locking
TREATMENT
- Rest. Continuing to throw with this problem may lead to major complications and permanently jeopardize a child’s ability to play.
- Strict throwing restrictions protect the elbow from further injury.
- Immobilization may be necessary in severe cases or if restrictions are ignored.
- If the elbow does not heal or the tissue becomes unstable or loose, surgery may be the best option.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Resume throwing at a minimum of 6-12 months.
- Focused training to improve throwing form is often necessary.
Elbow stability is crucial for throwing athletes. The ulnar collateral ligament (UCL) is the most important stabilizer for the inside of the elbow. With repetitive throwing, the UCL becomes stretched and develops small tears. This is painful and ultimately leads to instability in the elbow. Typically, the pain is on the inside of the elbow – just below the bony bump where medial epicondyle apophysitis can occur.
These injuries rarely occur with a single event or throw. They’re more common in older adolescents, but may occur in younger athletes as well. An MRI with contrast injected in the joint gives the best view of a tear.
The surgical reconstruction of the UCL is named after Tommy John, a baseball player who returned to major league pitching after having this procedure. This surgery doesn’t always lead to improved performance. Though many athletes do return to play after this procedure, preventing the injury is ideal.
SYMPTOMS
- Pain over the inside of the elbow with throwing
- Gradually increasing pain
- May feel unstable or “give way”
- Rarely popping
TREATMENT
- Rest for at least 6-12 weeks. Continuing to throw with this problem may lead to major complications and permanently jeopardize a child’s ability to play.
- Immobilization for 4-6 weeks followed by a hinged elbow brace.
- Anti-inflammatory medication.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Surgery is typically needed for complete tears or if the elbow is unstable.
- Focused training to improve throwing form is often necessary.
FEMALE ATHLETE TRIAD
 Female Athlete Triad is a medical condition that can affect girls and young women. It involves the following three components: energy availability, menstrual function and bone health. Clinical signs and symptoms may not all occur at the same time, so further evaluation is needed with the presence of any of these problems. Jane S. Chung, M.D., advises that education and early intervention are keys for young women with female athlete triad.
Female Athlete Triad is a medical condition that can affect girls and young women. It involves the following three components: energy availability, menstrual function and bone health. Clinical signs and symptoms may not all occur at the same time, so further evaluation is needed with the presence of any of these problems. Jane S. Chung, M.D., advises that education and early intervention are keys for young women with female athlete triad.
Changes in Menstrual Cycle
Young girls who are very lean, train a lot or do not have a well-balanced diet may start their menstrual cycle later than others. Some may start in a normal time frame. However, changes to diet and exercise habits may cause the cycle to be less frequent or stop during times of heavy training.
Eating Problems
Each athlete has a unique nutritional need to keep their body prepared for training, competition and normal growth. Sometimes, in an effort to achieve a specific weight or appearance, an athlete may restrict calories or make other choices to limit weight gain. Poor eating habits can lead to changes in several normal body processes. This can actually worsen performance, when an athlete is really trying to improve performance.
Osteoporosis or Weak Bones
Changes in hormone production that cause changes in the menstrual cycle lead to poor bone strength. A diet without proper amounts of calcium also causes bones to become weak. Therefore, athletes with eating issues are at high risk of injuries to bones. These often show up as stress fractures, small breaks in the bone that are difficult to detect but cause pain and require long rest from activity.
Hip
 The hip is a ball-and-socket joint with lots of soft tissue to help the bones stay together. Dancers, gymnasts, soccer players and ice hockey players move their hips in extreme motions over and over again, causing problems that can become progressively worse over time. Early recognition of signs and symptoms often results in very successful outcomes without surgery.
The hip is a ball-and-socket joint with lots of soft tissue to help the bones stay together. Dancers, gymnasts, soccer players and ice hockey players move their hips in extreme motions over and over again, causing problems that can become progressively worse over time. Early recognition of signs and symptoms often results in very successful outcomes without surgery.
Conditions we treat:
- Femoral acetabular impingement (FAI)
- Labral tears
- Snapping hip
- Hip and groin strains
- Overuse hip conditions (such as those seen in dancers and gymnasts)
- Pelvic apophysitis
- Pelvic avulsion fractures
KNEE
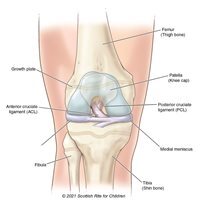 Knee injuries and their prevention in youth sports are hot topics. Young athletes have unique risk factors and require unique treatments. All growing bones have sensitive spots called growth centers that are filled with cartilage until the bone takes its final shape. Some growth centers are at risk of injury from running and jumping. Others that help our legs grow symmetrically and straight are at risk of being damaged from fractures or during surgeries for major ligament injuries. In these cases, a pediatric orthopedic surgeon has the expertise to make a plan for treatment and monitoring for the best outcomes.
Knee injuries and their prevention in youth sports are hot topics. Young athletes have unique risk factors and require unique treatments. All growing bones have sensitive spots called growth centers that are filled with cartilage until the bone takes its final shape. Some growth centers are at risk of injury from running and jumping. Others that help our legs grow symmetrically and straight are at risk of being damaged from fractures or during surgeries for major ligament injuries. In these cases, a pediatric orthopedic surgeon has the expertise to make a plan for treatment and monitoring for the best outcomes.
OSTEOCHONDRITIS DISSECANS
 The surfaces of the bones in the joints are covered with smooth tissue called articular cartilage. Osteochondritis dissecans (OCD) is a problem in this cartilage and the bone just beneath it. It occurs most commonly in the knee, elbow and ankle. Repetitive motions or overuse injuries in these joints put pressure on the cartilage and bones that cause injury over long periods of time.
The surfaces of the bones in the joints are covered with smooth tissue called articular cartilage. Osteochondritis dissecans (OCD) is a problem in this cartilage and the bone just beneath it. It occurs most commonly in the knee, elbow and ankle. Repetitive motions or overuse injuries in these joints put pressure on the cartilage and bones that cause injury over long periods of time.
We see OCD most often in 12-16 year olds. Though it can happen to anyone, we see this problem in athletes that perform repetitive motions like running, jumping, pitching or certain motions in gymnastics.
We’re unsure what causes this in some patients. It could be a change in the blood supply to the bone and cartilage. Sometimes an injury causes the changes. This is called an osteochondral fracture or injury.
SYMPTOMS
There may be pain in the joint that gets worse with activity. Or there may be symptoms like popping, clicking or swelling in the joint.
TREATMENT
In early stages, your provider may recommend rest and a brace to help the tissues recover on their own. In later stages, more aggressive treatments are required. Pediatric orthopedic surgeons, like Philip L. Wilson, M.D., and Henry B. Ellis, M.D., treat OCD with minimally invasive arthroscopy. The treatment is only necessary after a thorough investigation of the tissues with X-rays, an MRI or diagnostic surgery.
RETURN TO SPORTS
In many cases, activities like swimming, diving, biking, golf and yoga are good alternatives for young athletes. Our goal is to keep children active, but to protect joints that are at risk of long-term problems from overuse injuries.
SHOULDER
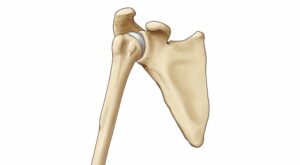 As a shallow ball-and-socket joint, the shoulder allows for a wide range of motion for overhead sports like baseball and volleyball. This range of motion also increases the risk of instability and injury to the joint. Repetitive motions or a single, forceful event may lead to tissue damage, resulting in changes to the shape of the bones and soft tissues. Many shoulder problems in young athletes are preventable. And early recognition often allows nonsurgical treatment with faster recovery.
As a shallow ball-and-socket joint, the shoulder allows for a wide range of motion for overhead sports like baseball and volleyball. This range of motion also increases the risk of instability and injury to the joint. Repetitive motions or a single, forceful event may lead to tissue damage, resulting in changes to the shape of the bones and soft tissues. Many shoulder problems in young athletes are preventable. And early recognition often allows nonsurgical treatment with faster recovery.
Our Experts
Taylor Dawson, P.A.-C.
Philip L. Wilson, M.D.
Henry B. Ellis, M.D.
John E. Arvesen, M.D.

Jane S. Chung, M.D.
Jacob C. Jones, M.D.
Shane M. Miller, M.D., FAAP
Kevin Chiang, M.D., M.Ed.

Ben Johnson, P.A.-C., A.T.C.

Chuck Wyatt, M.S., CPNP, RNFA
SPORTS NUTRITION
Our team is committed to caring for young athletes, even before they may need us. Scottish Rite’s certified sports dietitian works closely with this population to help them understand the importance of sports health and nutrition and fueling the body to stay healthy and in the game.
Latest news: sports medicine
AP News: Teenage Girls Are Most Likely to Tear Their ACLs
Last year, biomechanical researchers at Scottish Rite for Children began providing high school teams with resources typically only available or affordable at the professional and collegiate levels. They created pre-season injury-prevention trainings,…
Podcast: Balancing Training, Growth and Play
Sports medicine orthopedic surgeon John E. Arvesen, M.D., was invited to share his expertise on the right way to support a young athlete without pushing too hard on the Heaven or Heisman…
Kamryn Serves A Comeback After Knee Injury
Kamryn spends most of her time on the volleyball court, a sport she has loved since high school. She makes an impact at the net as a server for her college’s volleyball…
NBC 5: ACL Injuries Among Girls Are on the Rise
Movement science researchers at Scottish Rite for Children received a $1 million grant from Lyda Hill Philanthropies to fund, in part, a project that will tackle why teen girls tear their anterior…
Get to Know Our Staff: Ava Davis, Movement Science Lab
What is your job title/your role at Scottish Rite?I am a biomechanist for the Movement Science Lab (MSL) in Frisco. I help with a range of things, like collecting data, analyzing data,…
Noah Dunks on Osteochondritis Dissecans of the Knee
Cover story previously published in Rite Up, 2025 – Issue 3. by Kristi Shewmaker It happened after school. At an innocent game of touch football, Noah was tackled from behind. He never…
CBS Texas: How the Culture of Youth Sports Is Changing and Becoming More Accepting
A recent CBS Texas report explored how the culture of youth sports is shifting to prioritize fun, balance and emotional well-being over pressure and competition. Director of Medical Sports Medicine, Shane M.…
Frisco Style: When the Game Gets Too Big
By Monica Wallis In cities like Frisco, where the population has surged by over 77% in the last decade and sports are stitched into the community’s identity, the growth of youth athletics…
Scottish Rite for Children Announces World Champion Gymnast Skye Blakely as Its Health Care Ambassador
Scottish Rite for Children proudly welcomes Frisco’s own Skye Blakely, world champion gymnast and former patient, as its newest ambassador. Blakely will use her journey as an elite athlete to help spotlight…
Lyda Hill Philanthropies Awards Scottish Rite for Children $1 Million to Study ACL Injury Prevention in Young Female Athletes
Groundbreaking studies will address the ACL epidemic in active adolescent females by using movement science Movement science researchers at Scottish Rite for Children have received a $1 million grant from Lyda Hill…
Sign up to receive our digital newsletter with tips and insights for parents of young athletes