Ten Ways To Manage Pain Without Medication
Whether following an injury or a surgery, pain management is an important factor in many orthopedic conditions. Our psychology experts provide our patients with the necessary techniques and skills to manage their pain, preventing the need for extensive medications. Much of pain management is based on mental perception. Pediatric psychologists Emily Gale, Ph.D., L.P., ABPP, and Emily Stapleton, Psy.D., explain how to manage pain using psychology.
Importance of Pain Management
Nobody wants to be in pain, and ongoing or chronic pain can lead to mental health issues, such as anxiety and depression. Pain management is important to prevent increased stress levels and improve comfort in daily life. “Non-pharmacological pain management interventions are important because they allow patients to increase comfort for continued function, therefore supporting overall quality of life and allowing them to stay involved in the activities and sports they love,” Stapleton says. “Individuals who use these strategies also tend to rely on medications less, thus experiencing fewer side effects, decreased drug dependency and have reduced health care costs.”
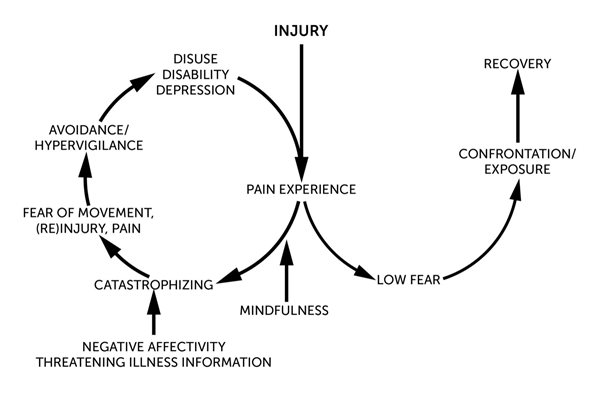
Emotions and Pain Management
Our emotions and behaviors can directly impact our perception of pain. “The experience of pain is a multifactorial experience in our brains — multiple centers, including the limbic system, which is involved in emotional processing, help us understand pain,” Gale says. “In fact, the International Association for the Study of Pain defines pain as ‘an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.’ Therefore, emotion management is a critical part of managing pain. Specifically, negative emotions often amplify the intensity of pain while positive coping skills can mediate the experience of pain.” Different psychology methods can allow patients to regulate their emotions and work through painful situations.
Pain Management Techniques
Our team of experts have many tips to help patients cope with pain. The following techniques can help manage pain:
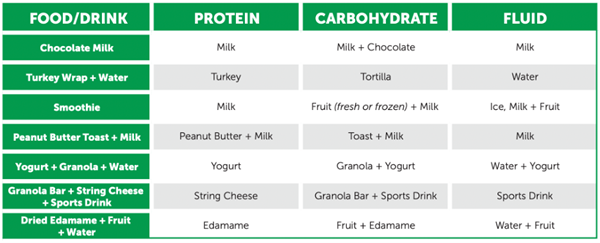
- Eat healthy meals at regular times throughout the day.
- Be sure to get plenty of sleep to refuel your body.
- Stay active and exercise regularly.
- Address any concerns with mood (i.e. poor mood, irritability).
- Use skills such as:
- diaphragmatic breathing
- progressive muscle relaxation
- guided imagery
- positive self-talk
- stress management
Diaphragmatic Breathing
Diaphragmatic (belly) breathing is a technique that strengthens the diaphragm while deeply breathing.
- Use the diaphragm and expand your belly instead of the upper chest muscles.
- Diaphragmatic breathing can help you relax, breathe more easily and strengthen your diaphragm.
Diaphragmatic breathing does not take the place of medicines or other treatments, but it can help you breathe more easily in certain situations. Learn how to use diaphragmatic breathing in our Pain Management Workbook.
Progressive Muscle Relaxation
Progressive muscle relaxation (PMR) or “Tense and Relax” is the simple practice of tensing, or tightening, one muscle group at a time followed by a relaxation and release of tension in that muscle group. Practicing this skill helps you get better at recognizing and reducing tension in your body and decreasing stress, anxiety and discomfort. PMR practice allows the muscles to relax more thoroughly after releasing, which makes letting go of physical tension more effective and increases relaxation.
Guided Imagery
Imagining a relaxing place or thinking relaxing thoughts can reduce pain and decrease stress. You can use imagery to imagine you’re somewhere else as a distraction from your pain and to feel more relaxed.
Positive Self-Talk
Self-talk is the inner voice or internal conversation that we have with ourselves. The way you talk to yourself can have a big influence on how you feel and act. Negative thoughts or self-talk increases stress, so with practice, you can learn to shift negative thoughts to positive ones and decrease stress using this cognitive-behavioral technique.
Learn more about the skills and psychology approaches used to manage pain in our Pain Management Workbook to assist patients and others with managing their pain. Download it now to get started. Learn more about our Psychology services.