In caring for the whole child, our team uses a multidisciplinary and multimodal approach to pain management. This means we go beyond prescribing analgesics (medicine for pain), in fact, we are actively working to eliminate the use of addictive opiods in our care.
A variety of approaches are used to prevent pain associated with a procedure. In addition to general anesthesia, nerve (hematoma) blocks are offered for some surgical procedures and fracture reductions. These have analgesic effects that can last up to 36 hours. Topical anesthetics are offered for invasive procedures including medication infusions and joint injections and aspirations.
Ambulatory nurse manager at the Frisco campus, Tabetha Rowe, R.N., says, “Not all patients have a procedure, but many of our patients present with musculoskeletal pain. Therefore, our guidance applies to most patients we see.” The ambulatory clinic, radiology and surgery staff provide education and resources to patients. Anyone can recommend or request that the provider make a referral to Child Life and/or Psychology for Scottish Rite patients that may benefit from additional assistance.
Non-Pharmacological Approaches to Pain Management at Scottish Rite
Patient and Family Education
With a new diagnosis and before and after procedures, relevant education is provided to ensure families understand the methods of pain control most appropriate to the situation.
- Protection, Rest, Ice, Compression and Elevate (PRICE) continues to be the gold standard to quickly offer an array of tools to address swelling and pain associated with an acute, and sometimes, chronic condition.
- Distinguishing between discomfort and pain is another point to address with patients and families. Some discomfort with an injury or after surgery should be anticipated, pain-free may not be a realistic goal to set for patients.
- Movement greatly reduces stiffness and muscle tension. This is the most important instruction for each patient. Moving as much and as often as is recommended based on the condition or procedure addresses comfort and risks of complications associated with inactivity, including stiffness and venous thromboembolism (blood clots).
- Getting enough quality sleep improves mental function and this can decrease sharpness of pain. Encourage eight or more hours/night.
- Optimal environmental factors can contribute to improved mood and may decrease the perception of pain. Open the shades and encourage interaction with others.
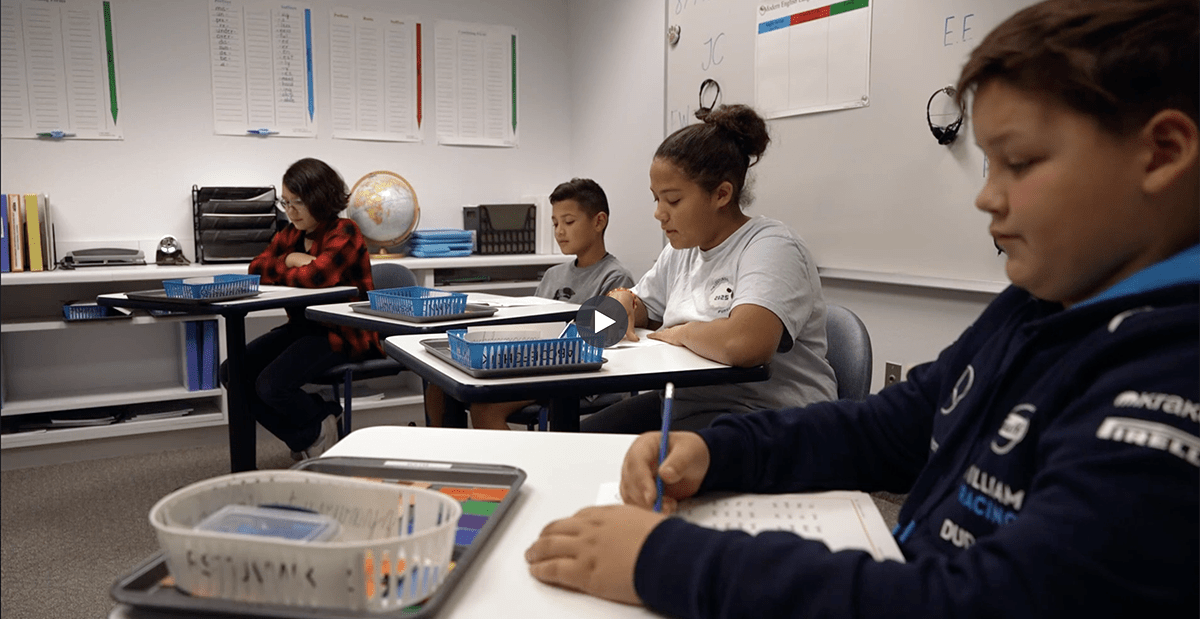
Child Life Specialists
Certified child life specialists are clinically trained to work with patients to reduce stress and anxiety during visits at Scottish Rite for Children. Child life specialist Laurie Hamilton, CCLS, explains, “Fear and anxiety can often be misinterpreted as feelings of pain. With preparation and support during procedures, patients can utilize appropriate coping plans to help with pain management..” Patients and families often tell us the child life specialist greatly helps to make the experience positive.
Here are some interventions child life specialists offer during a clinic, peri-operative or imaging visit.
- Age-appropriate explanation of the procedure or treatment can improve pain-like behaviors caused by fear and anxiety. This can also help the child focus on a coping plan that can help modulate pain.
- Providing pictures or an opportunity to see or touch equipment in advance may help a child understand the experience more accurately and be more confident with the plan of care.
- Advocating for the patient during a procedure helps the patient express feelings and find appropriate outlets for those feelings.
- Providing distraction techniques during the procedure encourages mental and physical relaxation which can help divert the child’s focus from the pain.
Pediatric Psychologists
Scottish Rite for Children recognizes the value of a psychological assessment and care in the treatment of children and adolescents. A consultation may be offered for several reasons, but may include discussing treatment decisions, a patient’s expressed need for psychological support or a formal mental health screening. Pediatric psychologists also help prepare patients and families for surgery.
Mental and emotional factors have been shown to influence outcomes of medical treatments, therefore, it is in the patient’s best interest to address those early in the treatment. Allowing the child to express feelings of fear, anxiety or other emotions can reduce stress associated with treatment or upcoming surgery. Pediatric psychologist Emily Gale, Ph.D., L.P., ABPP, says, “Untreated anxiety or depression can prevent engagement in the necessary steps for rehabilitation and recovery to return efficiently to their favorite activities.” Many times, the intervention is brief and aligns with phases of treatment and recovery. Gale says, “Managed early, the outcomes from a mental health perspective are good, and the physical recovery is frequently positively enhanced.”
The Psychology department offers clinic consultations, outpatient visits and referrals to resources in the community.
Pediatric Psychologist’s Perspective: Five Tips Managing Acute Pain in Children
- When introducing new medical terminology, always include an age-appropriate description.
- Help the child find words to describe their feelings of pain. This might include:
- Bruised feeling
- Tightness
- Soreness
- Aching
- Sharp pain
- Burning
- Stinging
- Numbness
- Pain and anxiety can become cyclical and can cascade into other feelings of fatigue and depression. Managing pain and discomfort before it starts is important. Use the techniques offered by the medical team proactively.
- Recognizing pain that is out of alignment with the condition or treatment can be a difficult process. Acknowledge the patient’s perceived pain while assessing for other risk factors of mental health conditions.
- Parents should model positive coping strategies, not only for pain, but for stress and uncertainty. Coping skills may include regular exercise, relaxation skills, breathing exercises, seeking social support, psychotherapy for mental health concerns and positive thinking.
Pain and discomfort cannot always be avoided. Proactive coping techniques to prevent prompt response, to escalating pain and using a multi-dimensional approach to will help to reduce the need for pharmacological analgesics, in particular opiods. As society continues to cope with opiod addiction, chronic pain and physical inactivity, our team is focused on getting kids back to childhood quickly, safely and without pain.
Find more resources for Medical Professionals.