Scottish Rite for Children has received one of Texas’ highest honors in health care quality — the Texas Hospital Association’s (THA) Bill Aston Award for Quality — for its innovative program that reduced opioid use by 28% in children undergoing spinal fusion surgery for scoliosis, setting an example for pediatric hospitals nationwide. The initiative successfully reduced opioid use without compromising pain management.
“This effort keeps kids safe by limiting opioid use while still delivering effective pain relief,” says Brandon A. Ramo, M.D., assistant chief of staff and chief quality officer at Scottish Rite for Children. “I’m proud of our team for leading the way with new solutions that will benefit children far beyond our institution.”
Established in 2010, THA’s Bill Aston Award for Quality recognizes hospitals across Texas that demonstrate exceptional and sustained improvements in patient outcomes through initiatives tied to national or state standards. This work reflects widely recognized priorities promoted by the Centers for Medicare & Medicaid Services, the Joint Commission and Texas quality improvement programs that focus on safer, higher-quality and patient-focused care. This is the second time Scottish Rite has received this recognition.
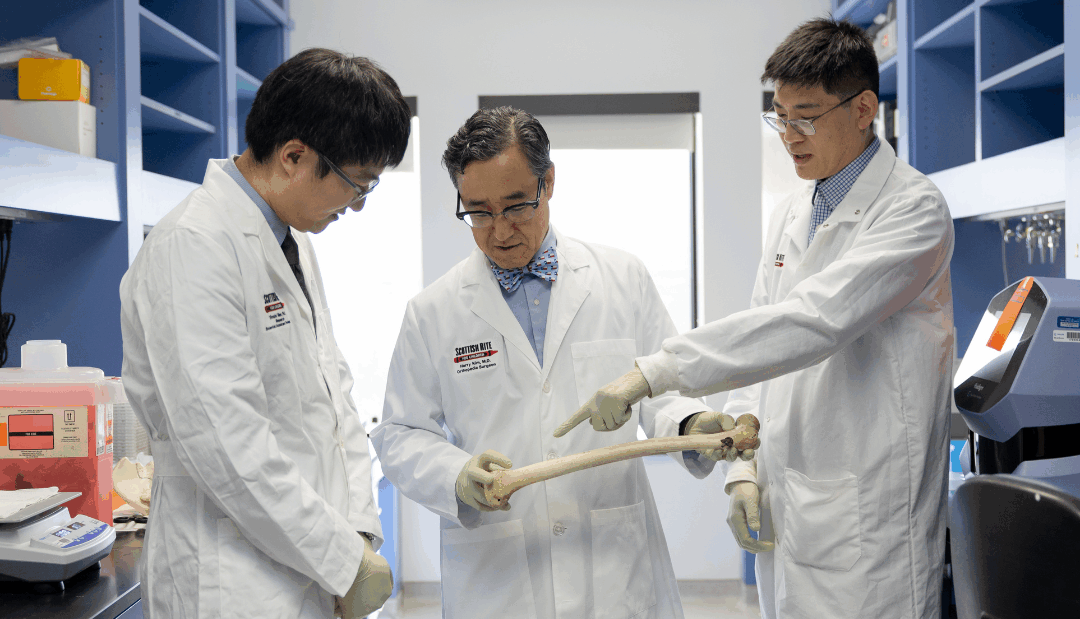
The award highlights the collaborative 8-year quality improvement project led by Ramo and Director of Quality Assurance and Performance Improvement Charu Sharma. The project is titled A Data-Driven Approach for Opioid Reduction Following Pediatric Spinal Fusion Surgery: A Model for Safe Pain Control. Ramo assembled a multidisciplinary team of doctors, nurses, pharmacists, quality experts and electronic medical records specialists to create evidence-based protocols designed to limit opioid intake in children safely.
“Receiving the Bill Aston Award for Quality is a tremendous honor and a reflection of the extraordinary teamwork at Scottish Rite,” says Scottish Rite for Children Chief of Staff Daniel J. Sucato, M.D., M.S. “This recognition reinforces our commitment to advancing pediatric care by improving safety, outcomes and quality of life for the children and families we serve.”
Using Plan-Do-Study-Act cycles — a step-by-step process of trying an idea, studying the results and making improvements — the team created new prescribing guidelines that helped adolescents recover from spinal surgery with fewer opioids.
Key elements of the project included educating physicians on the risks of overprescribing opioids, setting dosage limits while providing feedback to prescribers, empowering families with educational handouts on safe opioid reduction and promoting the use of non-opioid alternatives such as acetaminophen and ibuprofen.
“The program not only demonstrates measurable success in patient safety, but it also serves as a model for pediatric hospitals across the country, putting Scottish Rite for Children at the forefront of advancing pediatric patient care standards everywhere,” says Scottish Rite for Children President/CEO Robert L. Walker.