One-of-a-Kind Program Teaches Pediatric Fundamentals in Musculoskeletal Ultrasound
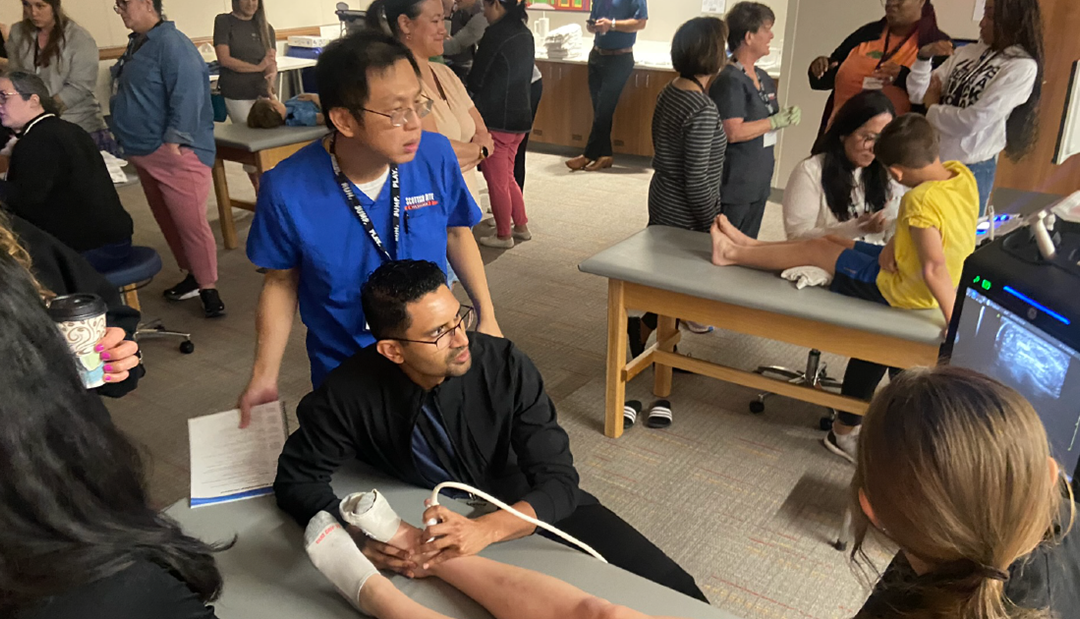
The use of musculoskeletal ultrasound (MSK US) is becoming increasingly popular and a point of emphasis in trainee education; however, most training programs focus on conditions in adults. Scottish Rite for Children experts have developed an introductory program to help new users learn about the unique skills and applications in the pediatric setting.
After a successful inaugural course in 2022, Scottish Rite hosted a second MSK US program. The feedback continues to show that we have a unique conference, and we plan to continue offering the program regularly.
This interactive, hands-on program features faculty from a variety of pediatric subspecialities including radiology, rheumatology and sports medicine. Attendees traveled to Frisco, Texas from across the country and internationally with a variety of clinical certifications including physical therapists, sonographers, nurse practitioners, physicians as well as radiology administrators.
Staff were encouraged to hear that all attendees indicated they were “very likely” or “definitely” going to recommend this course to others. Asked about the best part of the program, attendees’ responses are indicative of what future participants should expect:
- All the hands-on activities intermixed with patient lecture beforehand; the teachers were incredibly kind.
- Having pediatric patients!! Variety of faculty. Loved having MDS, RMSK, US Sonographer and radiologists. Truly a fantastic course.
- Short lectures alternating with hands-on
- Hands-on practice in SMALL groups with EXPERIENCED mentors.
- It was so helpful having pediatric models – I really learned a lot from the hands-on sessions!
- Multi-modal approach to learning
- The dual hands-on and lecture content kept my mind and body awake and elevated the overall learning experience!
Jacob C. Jones, M.D., RMSK, says, “The program is intended to offer an introduction to ultrasound basics including settings, scanning and injection techniques focused on skeletally immature patients.” Throughout the day, more than 20 children and teens ranging from 5 to 19 shared their time with our learners.
After a lecture introducing scanning for rheumatologic conditions, participants observed and practiced scanning patients with active joint inflammation. Nurse practitioner Heather Benham, D.N.P., APRN, CPNP-PC, RhMSUS explains, “We are grateful for these patients and the other children volunteers who make this course so special. It is very difficult to teach these principles when scanning healthy joints.”
During one scanning session, Scottish Rite sonographer Kelly Sherrard, RDMS, demonstrated the techniques of evaluating newborns for developmental dysplasia of the hips. Three-month-old twins served as our models for this exciting addition to the program. The expertise required for this population makes it difficult to include this training in the program, but attendees expressed their appreciation for the demonstration and the complexity of the skill.
Join the email list so you can gain early access to registration for future courses. Our next program is being planned for November 2023.