Sixteen-year-old Danielle is an innovator at heart. During her scoliosis treatment, she discovered solace in the hum of motors at her school’s robotics club. “Robotics helped me power through my treatment,” Danielle says.
When Danielle was in elementary school, she was diagnosed with adolescent idiopathic scoliosis (AIS) at Scottish Rite for Children. AIS is the most common form of scoliosis, affecting children ages 10 to 18. She had a lumbar, or lower spine, curve of 24 degrees. To prevent her curve from progressing, bracing was recommended.
Bracing is a common treatment method for children with scoliosis whose curves measure between 20 to 40 degrees. “Scoliosis was a new word to me,” Danielle says. “No one in my family had it. All I understood was that bracing would avoid the possibility of needing surgery. However, I was nervous about feeling different for wearing a brace.”
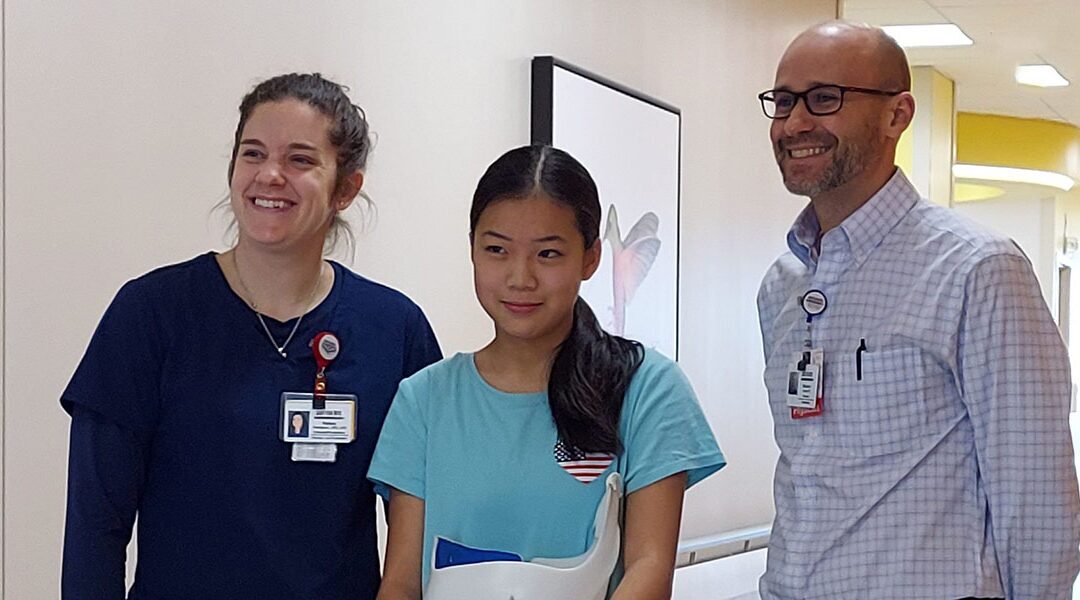
An expert clinical team guided Danielle through her spine treatment. Assistant Chief of Staff Brandon A. Ramo, M.D., monitored Danielle’s curve while Orthotist and Prosthetist Manager Kelsey Thompson, C.P.O., L.P.O., created and adjusted her brace. While it took time to adapt to wearing a brace, Danielle shares that her treatment brought her closer to her beloved passion of robotics in eighth grade.
“Once I joined the robotics team, the brace was no longer my focus,” Danielle says. “Robotics gave me something to look forward to everyday. I channeled all my energy into competing with my robotics team.”
After three and a half years of commitment, Danielle was cleared to stop wearing a brace. “The moment my treatment ended, it felt bittersweet,” Danielle says. “It was hard to say goodbye to Dr. Ramo and Kelsey, both of who I have come to know well during my regular check-ups. I am grateful to them for all the care they have given me.”
Danielle plans on taking her experiences at Scottish Rite and applying them to the world of technology. She mentors kids interested in robotics by helping them build the knowledge needed to improve, such as learning engineering, programming or marketing skills. Additionally, she maintains her Scottish Rite connection by being a peer support to other children undergoing bracing for scoliosis.
“Helping others is my way of saying thank you to Scottish Rite,” Danielle says. “Though my brace is gone, the strength, resilience and community I found will remain with me forever.
Do you have a story? We want to hear it! Share your story with us.