Gracee Gets Back in the Game After The Tether™ Spinal Surgery — the First at Scottish Rite
by Kristi Shewmaker
Gracee never imagined that one day she would play basketball in the Dallas Mavericks® practice gym, much less play one-on-one against her 6’5” pediatric orthopedic surgeon. As a 15-year-old high school varsity basketball player of Tuscola, she also never imagined that three months before that, she would be the first patient at Scottish Rite for Children to receive The Tether™ Vertebral Body Tethering System, a surgically implanted spinal device that is used to treat scoliosis.
Gracee grew up with basketball. “As a little girl, she went to the gym a lot because we were in the gym a lot,” says Carla, her mother. Gracee’s father, Hunter, is the high school varsity girls basketball coach. Gracee watched him coach her older sister before playing herself.
Gracee started playing competitive basketball in second grade. “We sent letters home to the girls in her class saying that we were going to meet one day a week to skill and drill,” Hunter says, “and it grew from there.” Throughout the years, Hunter coached Gracee and her team in various leagues. In middle school, Gracee joined her school team. In high school, Gracee started on the varsity team with some of the same girls that she has played with since second grade. “What I love most about basketball is the friendships that come with it,” Gracee says.
The summer before her freshman year, Gracee was seeing a chiropractor for an issue with her hip flexor, and Hunter mentioned that she had scoliosis during the appointment. A school nurse had noticed it during a routine screening when Gracee was in elementary school. Her curve was less than 10°, so her pediatrician had been monitoring it. “When she laid down on the chiropractor’s table, and I saw her back,” Hunter says, “I was like, ‘Oh my gosh!’ We didn’t realize to what degree the curve had gotten.”
Hunter contacted Scottish Rite for Children for help, and there, Gracee was diagnosed with adolescent idiopathic scoliosis. This condition occurs in patients ages 10 to 18, and the cause is unknown. Her curve measured 42°. “I was shocked,” Gracee says. “I didn’t think it would be that bad.”
Initially, Gracee wore a brace to prevent further progression and to try to avoid surgery. However, within months, her curve progressed to more than 50°, which experts call the surgical threshold — the point when surgery is recommended to stop a curve from getting larger. “In a certain subset of kids wearing their braces, the curve still progresses,” says Jaysson T. Brooks, M.D., pediatric orthopedic surgeon. “They have so much growth potential left, their spine overpowers the brace.”
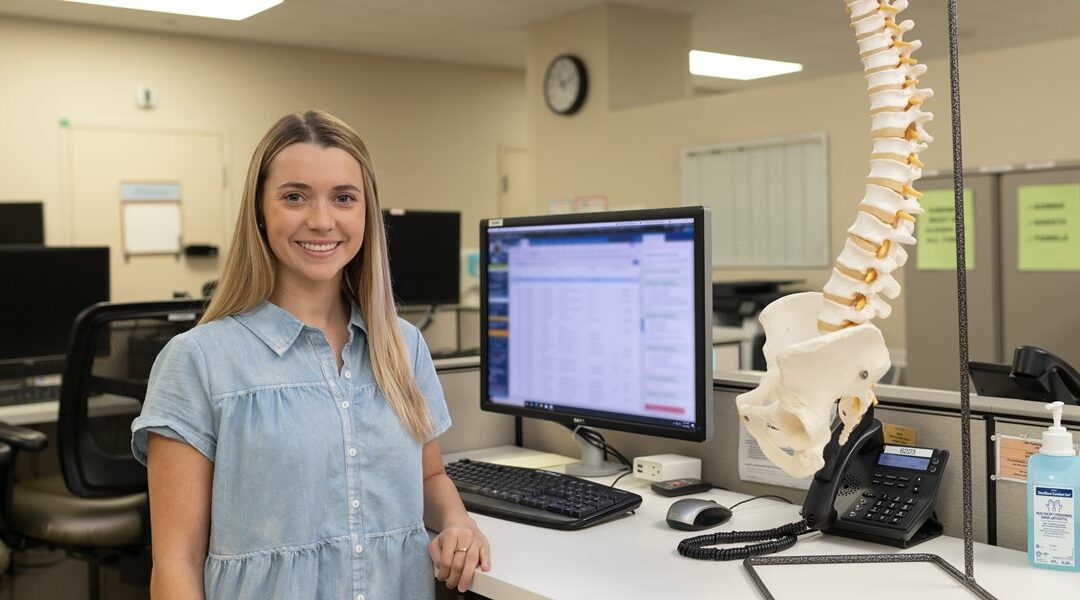
When Gracee and her family first met Dr. Brooks, they began discussing treatment options in anticipation of the need for surgery. Dr. Brooks presented two surgical options, including spinal fusion, which he calls “the gold standard treatment,” and The Tether™, a new non-fusion surgical device he had used previously to treat scoliosis but had not been used at Scottish Rite.
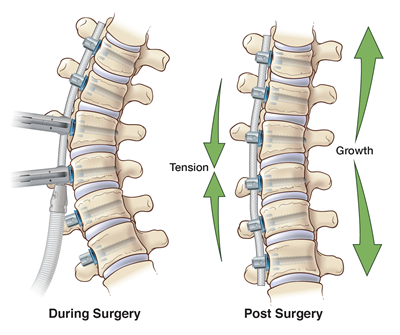
“Gracee was a good candidate for this procedure because her curve is flexible, and she was still really young from a bone standpoint, or skeletal maturity,” Dr. Brooks says. “The younger your skeleton is, the higher chance you have of getting taller, and using a tether requires you to be able to grow taller because it capitalizes on that growth.”
Over several appointments, Dr. Brooks discussed the pros and cons of each surgery, the difference in incisions, how X-rays look when rods versus a tether are attached to the spine, and the potential downsides and risks. “He did a really good job explaining the difference between the two,” Gracee says. “He also did a really good job of making me feel calmer.”
“There wasn’t a lot of anxiety on our part about which way to go,” Hunter says. “In my mind, vertebrae are meant to be flexible. If you can keep it the way God designed it, I think you’re better off. Obviously, there are times when the fusion is the only answer, but with this being another option, we wanted to try it.”
Gracee’s family chose this device because they wanted to maintain the overall flexibility of her spine as well as endure a shorter recovery period, so that Gracee could get back to playing basketball as quickly as possible.
“They are very intelligent and very pragmatic to approach a procedure that is this new and say, ‘I think this is going to be the right thing for my daughter,’” Dr. Brooks says. “They were mature enough as a family to say, ‘we’re okay with the potential consequences, but we think that the benefits outweigh the risks.’ You couldn’t have asked for a better family to be the first family for The Tether™ at Scottish Rite.”
“The whole time, I felt like she was in very good hands,” Carla says. “Dr. Brooks’ knowledge is one thing, but he is very compassionate and caring as well. I truly felt like he loved my child.”
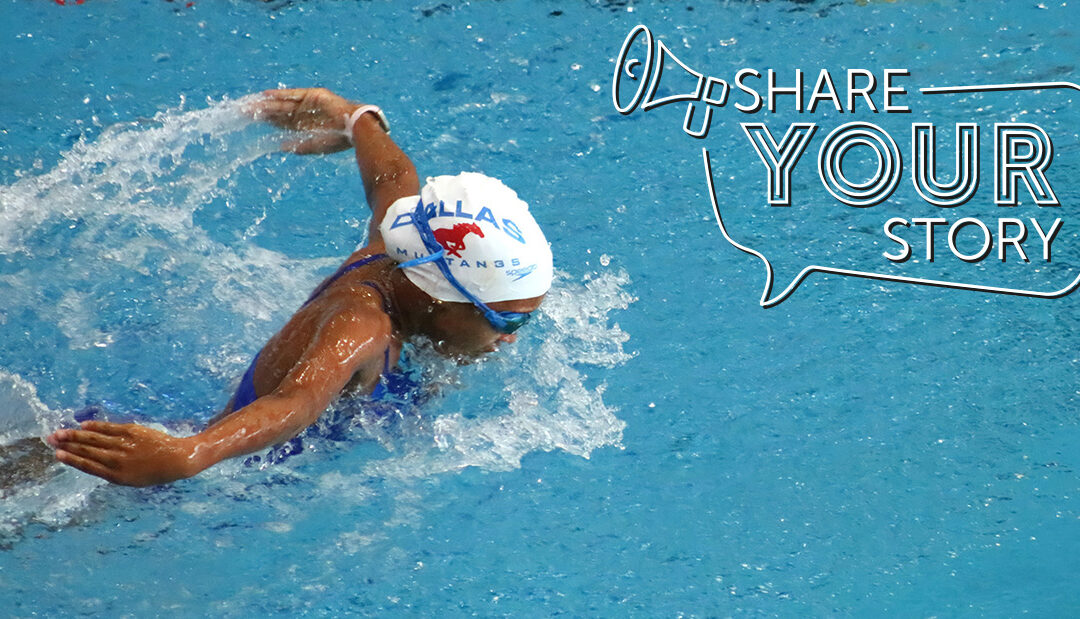
Two weeks later, Gracee went back to school. After six weeks, she played her first post-surgery game, and after three months, she found herself at the Dallas Mavericks® practice gym playing basketball with Dr. Brooks.
“It was a really cool experience,” Gracee says. “Dr. Brooks did pretty good.”

The feeling was mutual for Dr. Brooks. “It was a special opportunity for sure,” Dr. Brooks says. “I was pretty good at basketball in high school, but I’m super out of shape now. The only thing I had to my advantage was my height. Where she beat me in speed, I used my height.”
Gracee has played shooting guard for as long as she can remember. Hunter explains that she shoots in the 40% range from the three-point line. “Gracee’s a good shooter because she’s up at the gym at 5:00 or 5:30, three or four mornings a week working on her shots,” Hunter says. “Our basketball program is highly competitive. They’re ranked No. 2 in the state.”
In December, Gracee’s team won the Whataburger® Basketball Tournament, an invitation-only tournament in Fort Worth. When it was over, five players out of approximately 160 girls were chosen for the alltournament team. Gracee was one of the five.
“Going from being on a surgery table in April to being able to do that in December is just phenomenal,” Hunter says. “Gracee’s always been a spunky kid. There wasn’t much spunk a year ago, but we’re seeing it come back.”
“If Gracee had walked into my clinic with a 30° curve, she would not have gotten surgery because 30° isn’t big enough,” Dr. Brooks says. “In the end, if nothing changes, it’s still a win because she has a curve that is stable. There are lots of kids walking around with 30° curves who are living full, successful lives.”

Hunter says that they would be happy if her curve stayed where it is and ecstatic if it improves even more. “We’re just fortunate that we’re talking about a scoliosis curve that is manageable,” Hunter says. “When you see what other families at Scottish Rite are dealing with and the care that you see being administered to them, it’s as close to heaven on earth as you think you’ll ever see.”
“Everyone works so hard to make the kids at Scottish Rite feel at home, to make me feel at home,” Gracee says. “I wasn’t scared to be the first kid at Scottish Rite to get The Tether™. I like being groundbreaking. I like being the first.”
“And, our experience at Scottish Rite,” Hunter says, “has been nothing but first-class.”


.jpg?lang=en-US&width=200&height=181)