Groundbreaking studies will address the ACL epidemic in active adolescent females by using movement science
Movement science researchers at Scottish Rite for Children have received a $1 million grant from Lyda Hill Philanthropies to fund, in part, two projects addressing the concerning rise of ACL injuries in young female athletes. According to studies published in The American Journal of Sports Medicine, adolescent female athletes are at the highest risk of suffering an anterior cruciate ligament (ACL) injury: 29 times more likely than adult women and eight times more likely than their adolescent male counterparts.
The grant supports Scottish Rite’s initiative to find new ways to combat this ACL injury epidemic, and the studies it funds will leverage technology and clinical collaboration to identify effective prevention tactics. The team will look at how to reduce ACL injury risk in adolescent female athletes by tracking and syncing their menstrual cycles to a training program, and using the Movement Science Lab to simulate and test real-time decisions made in sports that may lead to or prevent injury. A portion of funds will also support overall injury prevention efforts.
“Because of this generous grant from Lyda Hill Philanthropies, our expert team is able to conduct vital research that will improve the care of young athletes,” says Scottish Rite for Children President/CEO Robert L. Walker. “We are grateful for the foundation’s support in this significant initiative to reduce sport-related injuries in young female athletes.”
Despite decades of research, significant disparities remain regarding ACL injury risk in female athletes. This problem has recently received international attention, and several institutions have begun to investigate the link between ACL injuries and the menstrual cycle in adult female athletes. However, few studies include adolescent female athletes, leaving a gap in the understanding of how hormone fluctuations affect how the body moves, performs and experiences the pressures of sport.
Under the leadership of Movement Science Division Director Sophia Ulman, Ph.D., the first study uses menstrual cycle tracking alongside neuromuscular training to better understand and adapt to the body’s physiological changes throughout the cycle. Early findings show that during the early follicular phase, right after menstruation begins, teen girls can experience up to a 42% increase in knee joint laxity, or looseness, which may raise their risk of ACL injuries by more than four times.
“Our last two years of preliminary work has highlighted how much research is still needed in this area,” Dr. Ulman says. “ With this study, instead of continuing to research why female athletes experience eight times more ACL injuries than males, we are asking, ‘How do we address this problem?’”
Participants in this study will track their menstrual cycle, allowing researchers to detect changes throughout different cycle phases. The neuromuscular training will adjust based on the cycle, using tailored strengthening exercises during the follicular phase and stability and balance exercises during the luteal phase, which is the second half of the cycle following ovulation. This approach targets phase-specific biomechanical risk factors unique to female athletes.
“Mirroring the rise in youth sports, especially at the competitive level, ACL injuries in the U.S. have doubled in the past two decades,” Dr. Ulman says. “The last 20 years of research into ACL injuries have clearly identified different outcomes based on the sex of the athlete. With this study, we aim to find a way to combat the higher injury risks seen in girls.”
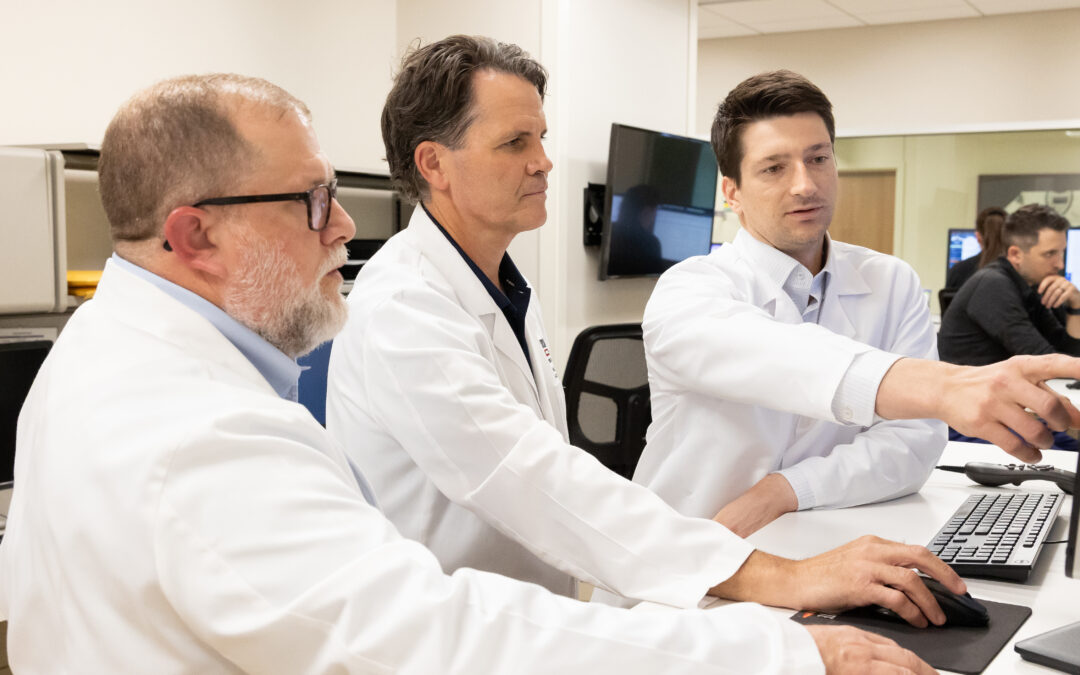
The research team also includes pediatric sports medicine surgeon and Medical Director of Clinical Research Henry B. Ellis, M.D., along with biomechanists, bioengineers and a physical therapist on the Movement Science team. In addition to their work at Scottish Rite, Ulman and Ellis hold faculty positions at UT Southwestern Medical Center’s Department of Orthopaedic Surgery.
“Young female athletes are at particularly high risk for serious injuries when playing competitive pivoting sports such as soccer and basketball,” Dr. Ellis says. “Our goal, through comprehensive multidisciplinary research, is to learn as much as we can about these injuries in hopes to provide families, coaches, athletic trainers and anyone involved in youth sports tools to prevent injuries in female athletes.”
The menstrual cycle study will recruit female high school athletes ages 14 to 19 who play basketball and/or soccer to participate in an eight-week preseason training program that will be led by their high school coaches and supported by Scottish Rite’s Movement Science staff. Taking place at their schools, which span the socioeconomic spectrum, girls will be tested both pre- and post-training to determine if the program reduces injury risk for the sports season.In the second study, researchers will use competition-like scenarios to identify modifiable biomechanical risk factors.
Young female athletes will be actively tested using alternating lights and actions during game-time scenarios, simulating the way the brain makes real-time decisions in competitive sport. Dual task exercises, such as memorizing color patterns while landing from a jump or moving in the direction of a light when it flashes, causes the athlete to make split-second decisions, like they would when deciding to pass the ball to a teammate during a soccer game. Scottish Rite’s team is studying how their body moves differently during these moments and how the athlete’s risk for injury may increase when their attention is divided. The data collected will help develop new rehabilitation protocols and return to play criteria, with the overarching goal of reducing the high rates of ACL reinjury.
To learn more about Scottish Rite’s Center for Excellence in Sports Medicine, please visit https://scottishriteforchildren.org/care/sports-medicine/.