Shouldering an Injury: What AC Joint Separation Recovery Looks Like
Young athletes can experience many shoulder injuries while playing sports, one of which being AC joint separation. Sometimes called shoulder separation, this injury affects the acromioclavicular joint, which rests where a part of the shoulder blade called the acromion connects to the clavicle, or collarbone.
If your child recently sustained an AC joint separation, you both are likely wondering how long it will take to recover and get back in the game. Athletes can usually return to sports and physical activities after 12 weeks. However, each child’s experience with AC joint separation is different. Your child’s recovery will depend on several factors, including how severe the injury is and the treatment your child receives.
Understanding AC Joint Separation
To understand the recovery process, it helps to understand what an AC joint separation is and how it impacts your child’s activities.
AC joint separation typically occurs when your child experiences a strong blow to the shoulder during a game or falls on his or her arm. The impact can strain or tear the ligaments attached to the underside of the clavicle — the AC and coracoclavicular (CC) ligaments — separating the collarbone and shoulder blade (scapula). Your child may have intense pain, swelling, bruising and limited range of motion in the shoulder and arm. Your child may also develop a bump above his or her shoulder.
Sports medicine specialists categorize AC joint injuries into several types, including:
· Type I injuries: These injuries are generally mild. The AC ligament is sprained, and the CC ligament is still intact.
· Type II injuries: These occur with a complete tear to the AC ligament, a sprain in the CC ligament and slight separation between the clavicle and acromion.
· Type III injuries: Both the AC and CC ligaments are torn, and the separation between the clavicle and acromion is more pronounced.
· Type IV, V and VI injuries: These involve tears in the AC and CC ligaments, and the clavicle is pushed further into the shoulder and neck.
Recovering From AC Joint Separation With R&R
An AC joint separation can often heal naturally using nonsurgical treatments, such as rest and temporary activity restrictions. Your child’s sports medicine specialist may recommend:
· Cold packs to reduce pain and swelling
· Immobilizing your child’s arm with a sling for resting the shoulder as it heals
· Medication for pain relief
Kids can often heal without surgery, even with severe AC joint injuries. Your child’s provider may start with conservative remedies before moving to surgery.
Surgery for AC Joint Separation
Surgery is generally used only with more severe AC joint injuries, and it may help if your athlete continues to experience pain despite nonsurgical treatment. Surgery can also help address bumps (deformities) that form after AC separation.
Surgical procedures involve removing a small portion of the collarbone to prevent it from rubbing against the acromion. Minimally invasive or open reconstructive surgery on the AC and CC ligaments may allow your child’s surgeon to reattach them to the collarbone. These procedures may involve plates or other materials to hold the ligaments in place.
Children who have nonsurgical treatments typically regain shoulder function within six weeks, while those who have surgery will have a longer recovery. Your child may need rehabilitation before returning to sports. Surgical recovery can take about six months.
Many children recover well from AC joint separation, and very few have complications.
AC Joint Separation or Clavicle Fracture?
Although older children and teenagers can experience AC joint separation, a more common shoulder injury in children is clavicle fracture.
Like AC joint separation, a clavicle fracture can occur after a hard fall or an impact from an accident. The two injuries cause similar symptoms, as well, including:
· A bump near the break
· A drooping shoulder
· Pain, swelling or bruising around the collarbone
· Pain that occurs when your child tries to move the shoulder or arm and that causes them to not use the arm as much as they normally might
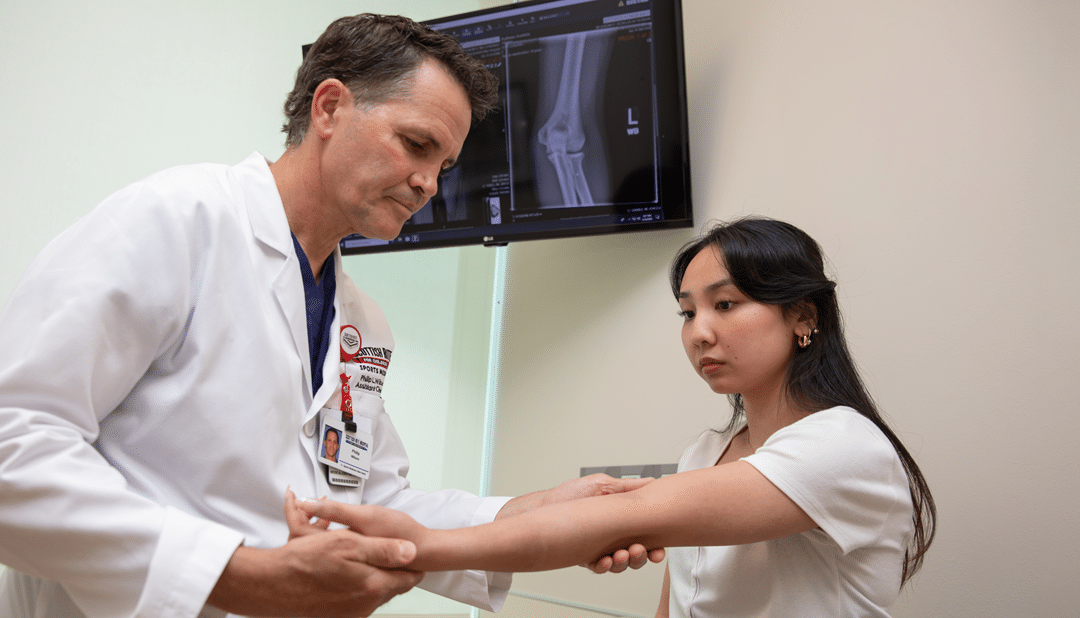
Your child’s provider may recommend imaging to determine whether your child broke a bone or experienced an AC joint separation. Fortunately, clavicle fractures, like AC joint separation, can often be treated without surgery.
Whether your child has AC joint separation or a clavicle fracture, it’s essential to follow the provider’s recovery instructions and ensure your child fully recovers before getting back to the field or playground.
At Scottish Rite for Children Orthopedic and Sports Medicine Center, pediatric orthopedic surgeons, physical therapists, athletic trainers, psychologists and other sports medicine specialists work collaboratively to develop personalized treatment plans for each young athlete. Call 469-515-7100 to learn about our sports medicine program.