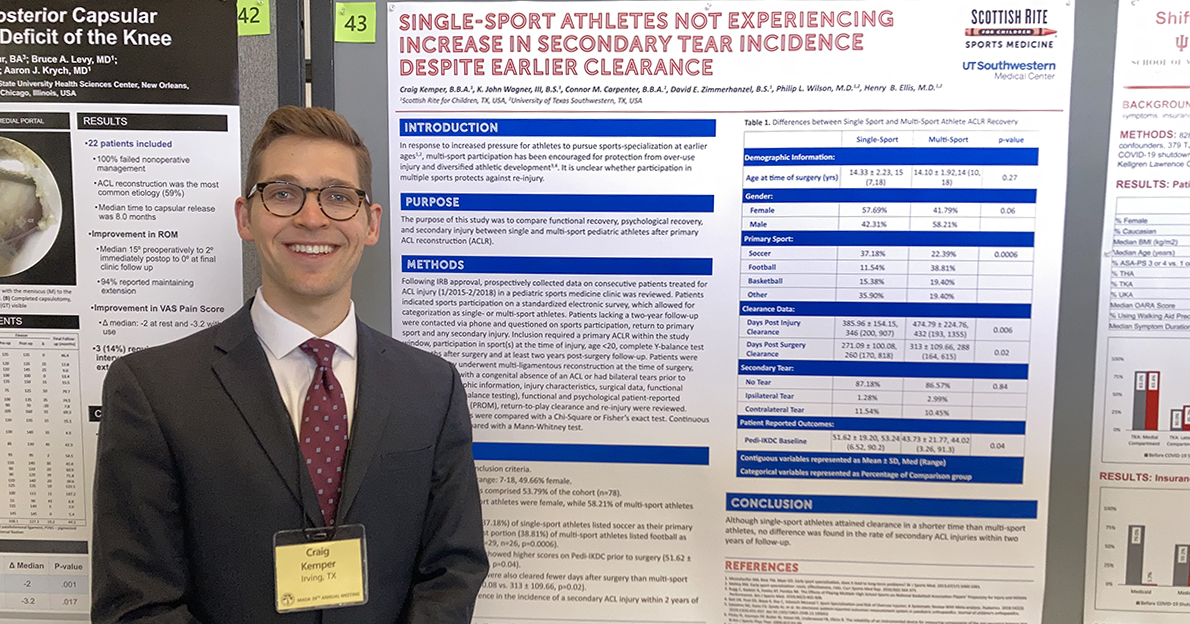
Anterior cruciate ligament (ACL) injuries, continue to challenge young athletes, many calling it an epidemic. Because of the high cost of care and loss of playing time, Scottish Rite for Children’s Sports Medicine team is actively looking for answers to prevent these...