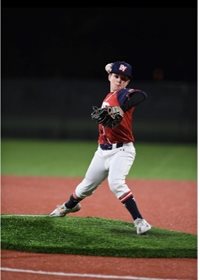
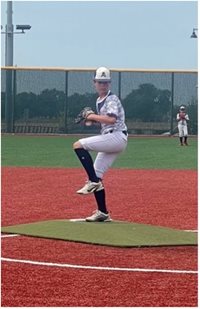
Movement Science – Breaking Down Movements in Young Baseball Players
As part of SAFE (Sports-specific Assessment and Functional Evaluation), our team is developing sport-specific protocols for the use of motion capture technology in sports medicine that are being used across the country. There are only a handful of sports that have received attention in the motion capture world, and those are typically performance-based models. The models that our team are creating evaluate foundational movements to help us predict injuries and improve return to play protocols. To do this, we will need to record a great deal of data from a large number of athletes.
For the past two summers, our Movement Science Lab team in Frisco has collected data sets on our baseball program participants and some other volunteers. Though we are just getting started on the total number of athletes to test, we are making great progress on tweaking the protocol and looking at preliminary results to understand where to go next. Here are a few things that we are looking at in the study:
Trunk mobility – specifically in the thoracic spine. We’ve identified the best way to capture the mobility of the upper spine. We believe that tightness there may affect the stress on the shoulder during throwing.
Motion throughout the body while throwing. Because our movement science lab is spacious, with 14-camera motion capture system, we can monitor joint angles, speed and forces throughout the body during high velocity pitching. We believe some movements are directly related to the development of elbow and shoulder injuries, particularly when there is a high volume of throws without rest.
Single leg stability with motion. Most sports require movement of the legs, and most of the time, only one leg is in contact with the ground. We are measuring the differences from side to side and between athletes to identify asymmetry in static and dynamic single leg movements. We believe asymmetry is a factor for increased injury risk in all athletes.
Leader of the project and assistant director of the Movement Science Lab in Frisco, Sophia Ulman, Ph.D., says, “Early results from this study are helping us to establish an evidence-based return to play decision-making model.” Many have heard of functional testing or return to play testing for athletes returning to sport after a significant knee surgery, such as an ACL reconstruction. This new upper extremity program is much needed in the pediatric sports medicine community. As we continue to collect information about healthy athletes, we will use the results to continue to modify the upper extremity return to play program. This is an example of where our clinical teams of physicians, physician assistants and physical therapists collaborate with our research team to make changes that impact athletes today.
We are continuing to work on this baseball project and invite healthy young athletes to help us. We schedule testing dates periodically and would be happy to send you the calendar to sign up or work with your team to find a date to do testing together.
To learn more about Movement Science, please call 469-515-7160 or email MSL.Frisco@tsrh.org.