Clubfoot Treatment: What Are Your Child’s Options?
If your baby is diagnosed with clubfoot, your first question may be, “What can we do?” Fortunately, effective nonsurgical clubfoot treatment options are available, and most children don’t need an operation. A pediatric orthopedic surgeon can help you decide what treatment makes the most sense for your child.
The Basics of Clubfoot Treatment
One of the most common foot-related deformities that may be present at birth, clubfoot occurs when your child has an inward-turned, high-arched foot. It isn’t painful for your baby, but if left untreated, the condition can lead to foot pain in the future. In addition, untreated clubfoot can cause an abnormal gait and restrict activities later in childhood.
Usually beginning soon after birth, clubfoot treatment can provide correction to the condition, so your child’s foot will have normal function, and your child will be able to walk without pain. With a pediatric orthopedic surgeon’s help and your commitment to following the treatment plan, clubfoot doesn’t have to be a permanent deformity. Treatment can help prepare your baby to walk, run, jump and skip through childhood.
The Ponseti Method: The Gold Standard of Nonsurgical Clubfoot Treatment
For many babies, correcting clubfoot involves a multi-step treatment called the Ponseti method, which is named after the orthopedic surgeon who pioneered it. This treatment starts with stretching and casting.
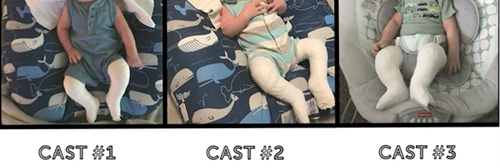
Over four to five weeks, your child will see a pediatric orthopedic surgeon for weekly manipulations. This gentle stretching gradually moves the foot into the correct position. After each session, the surgeon will apply a full-leg Ponseti cast to help the foot maintain its position.
A tight Achilles tendon contributes to clubfoot, and most patients receiving the Ponseti method have an Achilles tenotomy procedure. This procedure is quick and simple, is done in the clinic and is not major surgery.
With local anesthesia numbing the back of your child’s ankle, his or her orthopedic surgeon will cut the Achilles tendon to loosen it. The cut is so small and precise that it won’t require stitches. Afterward, your baby will wear a cast for three weeks while the tendon heals to the correct length.
Clubfoot can return, even with treatment. Your child will have to wear a brace with a metal bar attached to special shoes for four years. He or she will start out wearing the brace 23 hours a day. Once your baby begins pulling to stand the brace is used during nighttime hours only until it’s time to stop bracing.
The French Method of Clubfoot Correction
The Ponseti method isn’t right for every child. In some cases, another nonsurgical clubfoot treatment, the French method, may be a better fit. For this treatment, you’ll work closely with your child’s orthopedic surgeon and a physical therapist.
- The physical therapist will teach you how to gently manipulate, tape and splint your child’s foot, which, over time, moves it back into the correct position. You’ll repeat this routine daily for three months.
- After three months, your baby will likely need to have an Achilles tenotomy to release the tendon.
- Following the tenotomy, you’ll resume manipulating, taping and splinting the foot each day until your child reaches age 2 or 3. Your pediatric orthopedic surgeon will monitor your child’s progress and let you know when you can stop the daily regimen.
Treating clubfoot takes dedication, but the payoff is worth it. Your effort can set your child up for a lifetime of activity without foot pain.
Wondering what’s next for your baby after a clubfoot diagnosis? Schedule an appointment with a foot and ankle specialist who can recommend a treatment plan.