
Calling All Nurses: Volunteer at Scottish Rite for Children Camps
Scottish Rite for Children’s patient-centered care stems from its focus on helping patients navigate their conditions outside of the clinic. The Therapeutic Recreation department offers multiple specialized camps throughout the year, which are designed to teach patients how to live active and independent lives.
Camps bring together children with similar conditions in an environment that fosters friendships and lifelong memories through outdoor activities and games. The following camps are offered at Scottish Rite:
- Camp Joint Adventure: For patients between the ages of 7 to 15 who are diagnosed with arthrogryposis, multiple limb loss or various rheumatic conditions.
- Camp TLC: For patients between the ages of 9 to 16 who are diagnosed with spina bifida.
- Hand Camp: HD 1 is for patients between ages 5 to 9 who have upper limb differences. HD 1.5/2 is for patients between the ages of 10 to 17 with hand differences.
What makes Scottish Rite camps special are not only the uniqueness each child brings but also each volunteer’s commitment to providing a “can do” environment. Camps are supervised by counselors, which includes Scottish Rite staff members and volunteers.
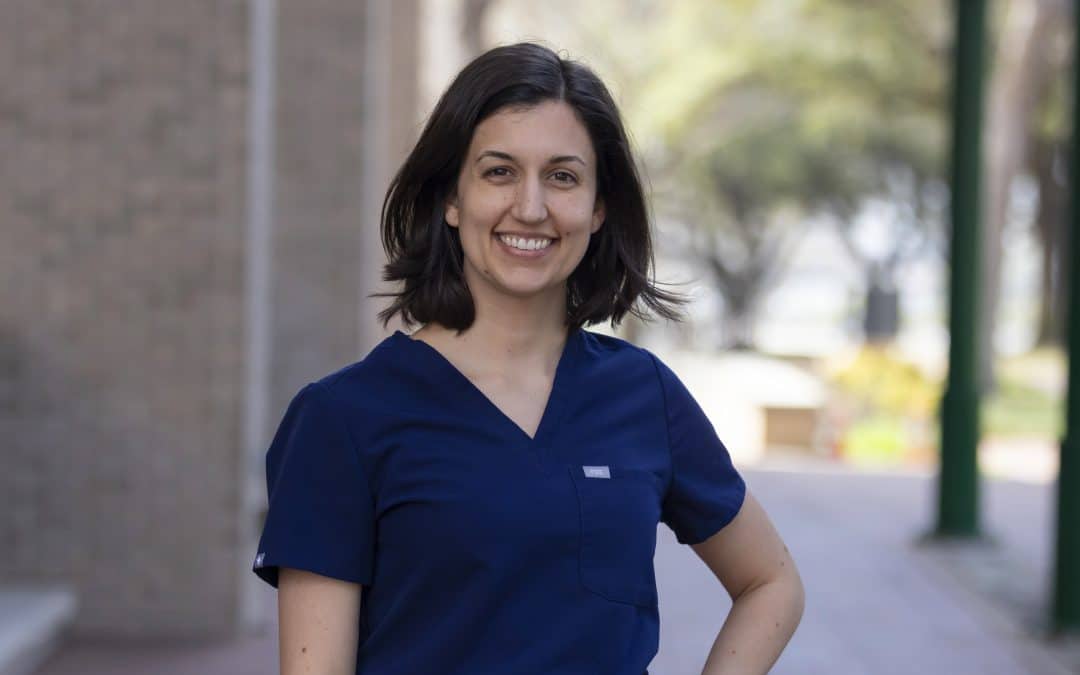
“A week at camp is not like any typical week as a nurse,” says Sheila Maldonado, R.N., who volunteers at Camp TLC. “On top of providing the fun for all our campers, counselors make sure they are healthy and safe during the entire experience. For nurses, it’s the best way to sharpen the skills we might not have used since school, while creating the most rewarding memories.”
All campers must be active patients of Scottish Rite. For staff members, many find that volunteering as a counselor is a unique way to interact with patients in a nonclinical setting.
“The best part about camp is seeing the connections made,” says R.N. Manager Alejandra “Alex” H. Medrano, M.S.N., R.N., who has volunteered for more than 20 years at Camps TLC and Joint Adventure. “They get a chance to build peer support networks. They also become more comfortable with their care team during appointments.”
The camps offered by Scottish Rite serve its mission of giving children back their childhood, allowing them to experience the joy of summer camp with their peers. “My favorite part is how inclusive these camps are and watching kids just be kids, including all the smiles, laughs, friendships and fantastic activities,” says Karol Yeager, R.N. “Out of all the activities, I think either the Slip ‘N Slide® or the zip line was my favorite to watch. The sheer joy from these kids that possibly have never done these things before was priceless!”
Camp TLC is currently accepting applications for campers and medical volunteers (cabin nurses). If you are interested in volunteering, please view the Camp Volunteer application process for more information.
To learn more about the application process, camp dates and more for Camp Joint Adventure and Hand Camps, please view our Camps page here.


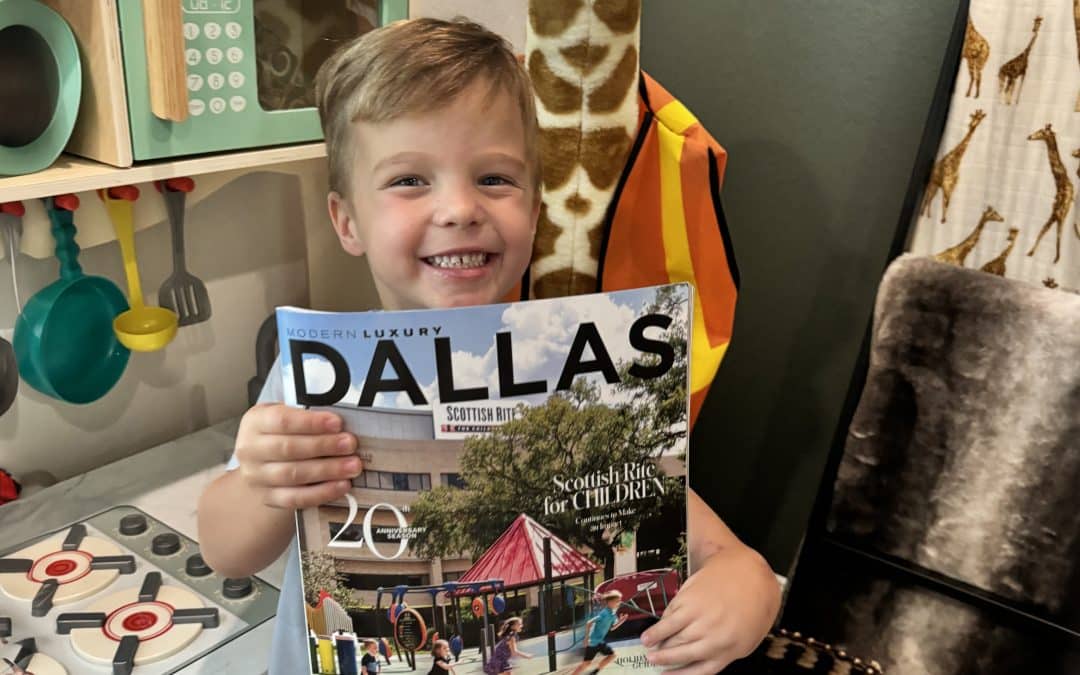
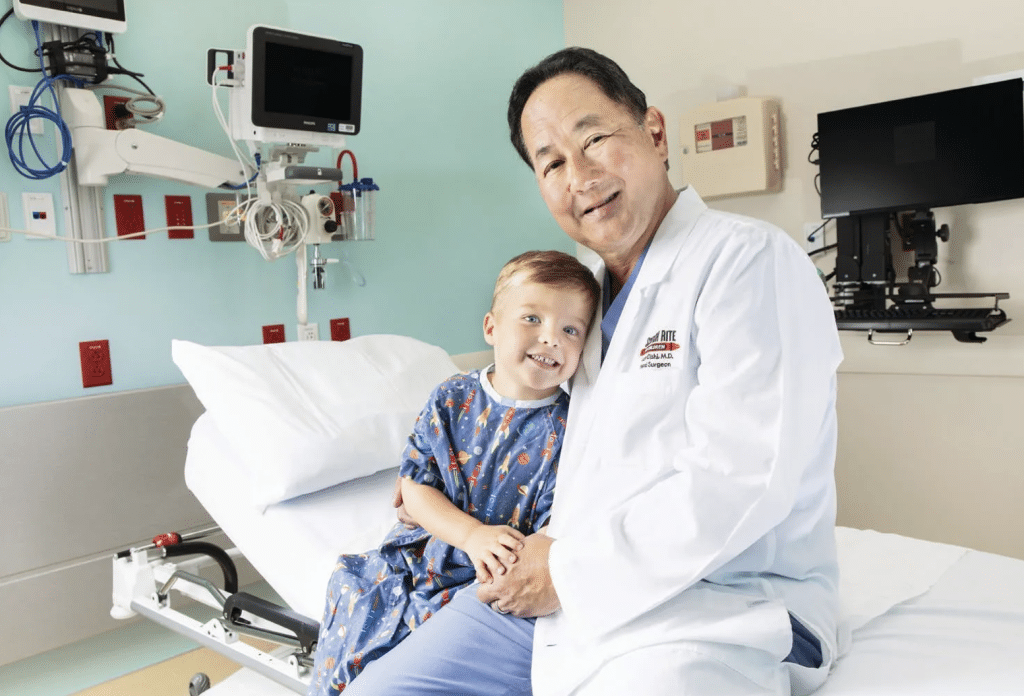 the eye and seek to understand their needs to best serve them. We give children back their childhood.” Having been a treasured staple within the North Texas community for over a century (established in 1921), Scottish Rite for Children continues to soar as a world-renowned leader in treating pediatric orthopedic conditions, and its patients are traveling here from all over the map. “Not only does Scottish Rite have a strong presence in the Dallas community, but it is also known for its excellence in patient experience nationally,” shares president and CEO for Scottish Rite for Children’s Bob Walker. “This year, NRC Health honored Scottish Rite for Children with the Excellence in Patient Experience Award for the eighth time in the nationwide pediatric category. Honorees are recognized for their efforts to consistently deliver outstanding patient experiences.” And, deliver they certainly do—with grace and gusto. From scoliosis, clubfoot, hand differences, and hip disorders, the compassionate team of experts’ unwavering commitment to children goes beyond the physical sense. They adhere to address three critical pillars for every child— the body, mind, and spirit. Offering a bevy of individualized therapies with inimitable in-house specialists, every child receives a regimen tailor-made to them. An additional component to adding a sense of playfulness to keep children in good disposition, the hospital hosts a myriad of recreational programs and specialized sports. With three locations within North Texas, the Dallas location is the largest—871,000 square feet perched on 15 acres of land.
the eye and seek to understand their needs to best serve them. We give children back their childhood.” Having been a treasured staple within the North Texas community for over a century (established in 1921), Scottish Rite for Children continues to soar as a world-renowned leader in treating pediatric orthopedic conditions, and its patients are traveling here from all over the map. “Not only does Scottish Rite have a strong presence in the Dallas community, but it is also known for its excellence in patient experience nationally,” shares president and CEO for Scottish Rite for Children’s Bob Walker. “This year, NRC Health honored Scottish Rite for Children with the Excellence in Patient Experience Award for the eighth time in the nationwide pediatric category. Honorees are recognized for their efforts to consistently deliver outstanding patient experiences.” And, deliver they certainly do—with grace and gusto. From scoliosis, clubfoot, hand differences, and hip disorders, the compassionate team of experts’ unwavering commitment to children goes beyond the physical sense. They adhere to address three critical pillars for every child— the body, mind, and spirit. Offering a bevy of individualized therapies with inimitable in-house specialists, every child receives a regimen tailor-made to them. An additional component to adding a sense of playfulness to keep children in good disposition, the hospital hosts a myriad of recreational programs and specialized sports. With three locations within North Texas, the Dallas location is the largest—871,000 square feet perched on 15 acres of land.




