Nutrition for Injury Recovery in Young Athletes
Nearly 60 million American children play sports, and many of them experience sports injuries. If your child gets injured, the path to healing starts in the kitchen. Proper nutrition for injury recovery may help your child spend less time on the sidelines. The key is knowing which foods to choose.
Foods to Avoid After an Injury
Sports injuries force athletic kids to do one of their least favorite activities: sit around. As they watch their teammates run back and forth, children may forget about habits that keep them on their game. Instead of healthy eating, they may want to fill up on unhealthy snacks and sweets.
Don’t let your children fall into this trap. Encourage them to eat the same foods they rely on when playing sports to ensure the best nutrition for injury recovery.
After a sports injury, your child should avoid the following:
-
Inflammatory foods. White bread and pastries are refined carbohydrates, which have much of their nutritional value stripped away. They are also associated with inflammation, which slows the healing process. Similarly, saturated fats found in butter, full-fat dairy, fried foods, and red and processed meats can raise inflammation but don’t offer additional nutrition value.
-
Sports drinks. Full of electrolytes, sports drinks help your child rehydrate when they sweat excessively during activity. While your child is resting and recovering from injury, however, sports drinks are just another sugary drink. Like refined carbs and fried foods, sugar is associated with inflammation.
Proper Nutrition for Injury Recovery
To help your injured athlete maintain muscle mass, feed them healthy, nutrient-dense foods, including:
-
Complex carbohydrates. Along with providing energy for your body to heal, complex carbs are full of vitamins and minerals. Good sources of complex carbs include lentils, brown rice, quinoa, and whole wheat breads and pastas. Rotate these different options into evening dinners to add variation to your family meals.
-
Fruits and vegetables. The vitamins and minerals found in fresh produce have many benefits. They heal wounds, aid in tissue growth and repair, and more. Fill your child’s plate with a variety of fruits and vegetables. Find various ways to prepare and present produce to keep things interesting. Dust vegetables with exotic spices like turmeric or crumble berries over Greek yogurt for a creamy afternoon treat.
-
Healthy fats. Eating healthy fats gives your child an energy boost. Additionally, healthy fats can have anti-inflammatory properties. Add healthy fats to your child’s diet by offering flax or chia seeds, avocado, or fish. Make these options intriguing by mixing avocado into a spicy guacamole or blending chia seeds into a fruit smoothie. When cooking other foods, use olive or sunflower oil for even more healthy fat.
-
Lean sources of protein. Protein intake protects against muscle loss. Foods rich in protein include lean meats, fish, low-fat dairy products, and nuts and seeds. Think turkey sandwiches, peanut butter toast and grilled chicken over colorful vegetables. The amount of protein your child needs varies, so talk with their provider to determine the right amounts during injury recovery.
-
Water. Complete nutrition for injury recovery requires hydration to help joints heal. Encourage your child to drink lots of water. To add bright flavor to your child’s beverage, consider spritzing it with slices of lemon or other types of citrus fruit.
Let your child help you as you prepare their meals and snacks. You may even consider using your child’s time off from athletics to plant a garden filled with fruits and vegetables they can enjoy throughout the year. Building healthy dishes together helps your athlete stay connected to their wellness as they recover. It is also a great opportunity to set and achieve goals as a family.
A Word on Concussion Nutrition
When young athletes experience a sport-related concussion, they also seem to benefit from proper nutrition for injury recovery. Research has shown that certain nutrients may benefit children after a concussion. They include:
-
Protein
-
Magnesium
-
Omega-3 fatty acids
-
Vitamin D
Additional research is needed on the effects of nutrition on concussion recovery. These nutrients can be found in many healthy foods but talk with your child’s provider before giving your child any supplements after a concussion.
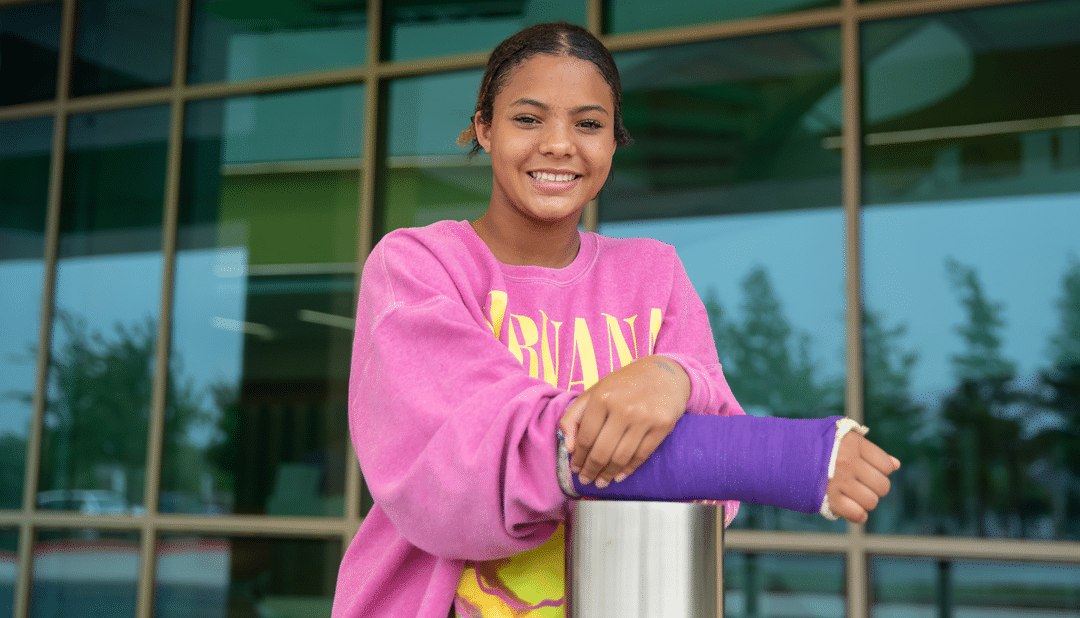
Is your young athlete sidelined with a sports-related injury? Our expert team at Scottish Rite for Children is ready to get them back in the game. Call 469-515-7100 to learn about our sports rehabilitation services.