ACL Injuries and Female Athletes: What You Need to Know
At Scottish Rite for Children, our sports medicine team cares for many young athletes with anterior cruciate ligament (ACL) injuries every year. With her previous experience as a Division II soccer player, sports physical therapist Nicole Shivley has a passion for finding ways to prevent injuries in female soccer players.
Keep reading to learn why ACL injuries occur more often in female soccer players and what they can do about it.
How do ACL injuries occur in soccer players?
Most ACL injuries in soccer are related to contact injuries. However, some are non-contact related and can occur from a sudden change of direction. For the most part, these non-contact injuries can be prevented. When a young athlete suddenly changes direction to evade an opponent or to avoid a play, their foot plants forcefully and abruptly. The subsequent “push off,” typically with a turn, puts a significant amount of stress on the ACL. This happens when the athlete’s body turns, but their knee or foot does not. Higher levels of aggressiveness, competition and speed only add to an athlete’s risk of injuries.
Why do young female athletes have a higher rate of ACL injuries in soccer than male athletes?
While the answer is still unknown, it is likely that a complex combination of factors causes ACL injuries in women, such as anatomy and movement patterns that are unique to young female athletes.
A specific posture, called genu valgum or knocked knees, is often found in adolescent girls. This posture may be due to the way the athlete’s bones have grown. Experts find that this is from poor movement pattern, which results from muscle weakness and poor control of the hips and legs. The position puts more stress on the ACL, particularly with activities like soccer.
Additionally, girls tend to have more strength in the muscles on the front of their thighs, the quadriceps (quads), than the muscles on the back side (hamstrings). This is referred to as “quad dominance,” and this imbalance directly affects how the knee functions during deceleration and changes in direction.
Lastly, hormonal changes across a young female athlete’s monthly menstrual cycle affects joint mobility and stability. ACL injuries can be caused from these fluctuations, contributing to certain weeks having higher or lower risk of injury throughout the month.
Is there any way to prevent an ACL injury in soccer?
Young female athletes can reduce their risk of experiencing an ACL injury by addressing certain areas in their body with exercise. These ways include:
- Strength training of the correct hip and knee muscles.
- Improving mechanics at the hip and knee during all movements.
- Correcting dynamic movement patterns, such as sprinting, decelerating and quick changes.
How do young athletes get started with strength and conditioning?
- Teams may have programs set up. Check with your athletic trainer or coach.
- Look for a local gym or program, such as our athlete development program, with appropriate supervision and guidance available for young athletes.
Here are some things to look for in any strength and conditioning program:
- Certified strength and conditioning (CSCS, ACE, etc.)
- Age and developmentally appropriate programming.
Young female athletes can also protect their bodies by ensuring they are taking care of themselves outside of their sport. These ways include:
- Rest when your body says it needs it.
- Respond to aches and pains. Early recognition and response can limit time on the bench.
- Integrate strength training in your weekly schedule.
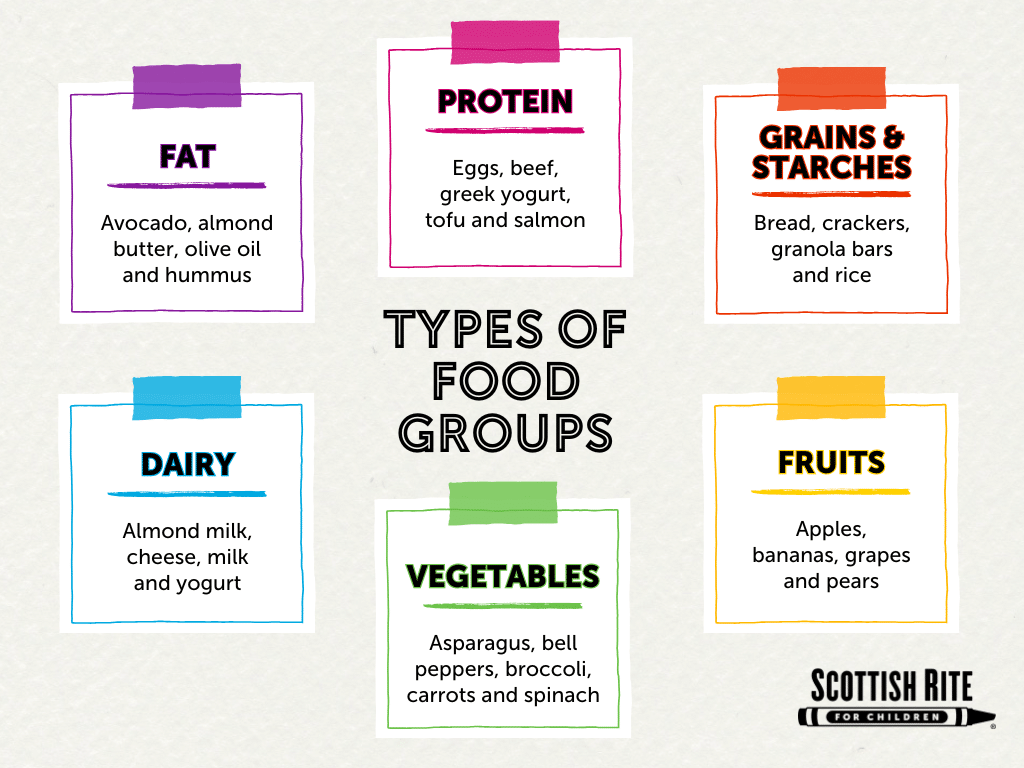
- Eat enough to keep up with your energy expenditure.
Strength and condition programs provide young female athletes with guidance on how to build a healthy body. Learn more about athlete development Scottish Rite for Children.