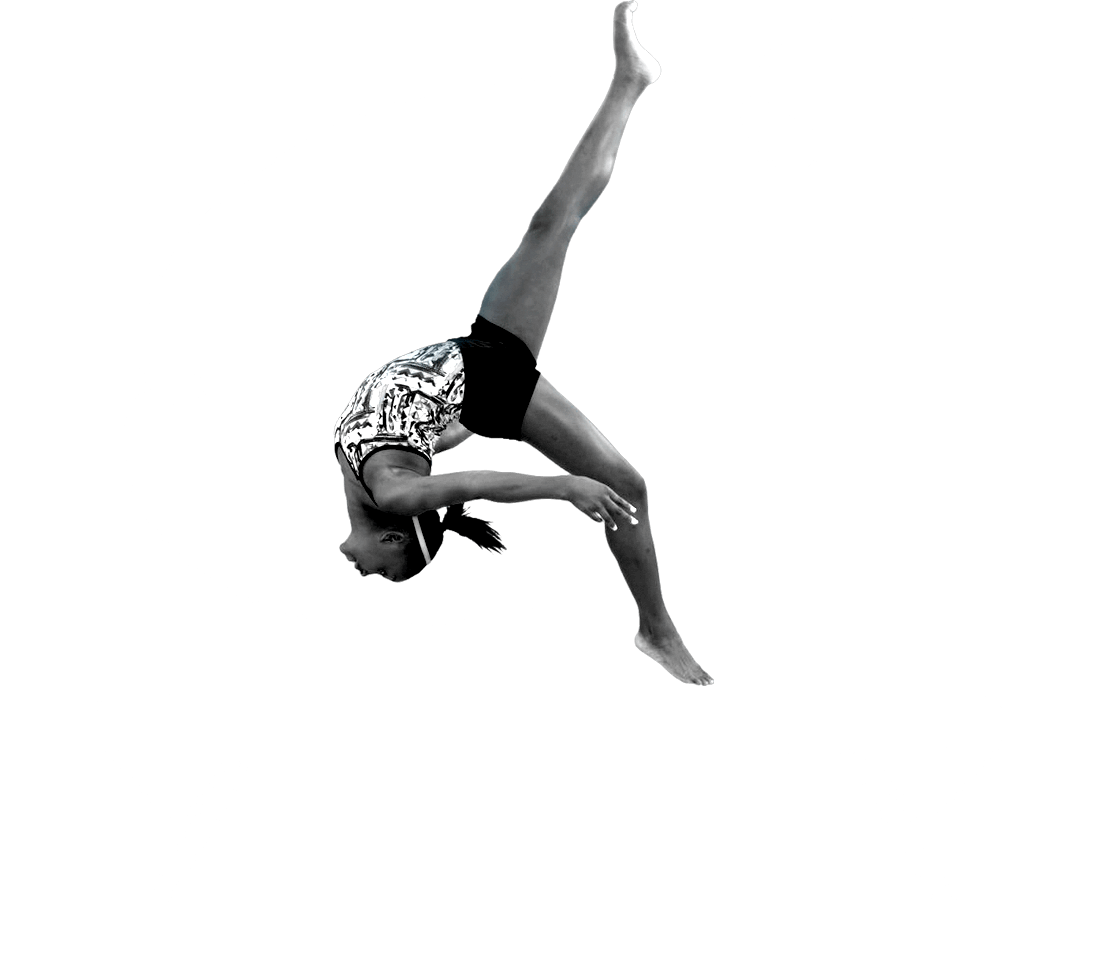
Sports Knee

KNEE CONDITIONS & TREATMENTS IN YOUNG ATHLETES
Read more about the pediatric sports medicine services we provide.
KNEE CONDITIONS
KNEE
-2022-01.jpg?width=750&height=771&ext=.jpg)
- Anterior cruciate ligament (ACL) tears
- Posterior cruciate ligament (PCL) tears
- Collateral ligament tears
- Meniscus tears
- Discoid meniscus
- Cartilage conditions such as osteochondritis dissecans (OCD)
- Knee Contusion
- Patellofemoral (Kneecap) Instability and Dislocations
- Tibial spine fractures
- Osgood-Schlatter disease
- Patellofemoral Pain
- Sinding-Larsen-Johansson (SLJ) Syndrome
A ligament is a strong band of soft tissue that connects two bones together. The anterior cruciate ligament is a main stabilizer inside the knee joint. The ACL prevents hyperextension (over-straightening) and extreme rotation in the knee, which can be caused by a collision or sudden change in direction. These very strong forces can partially or completely tear the ACL.
SYMPTOMS
- Knee pain and difficulty walking•Swollen knee (joint effusion)
- A “pop” heard or felt at the time of injury
- Knee instability or a feeling of “giving way”
PREVENTION
DIAGNOSIS
TREATMENT
Because the re-injury rate after an ACL injury is concerning, our team takes the decision of returning to sports seriously. Among other tools and milestones, we utilize the Y-Balance Test [link to YBT video on YouTube] to help determine an athlete’s readiness to return to sports. Though it can take 9-12 months for an athlete to return to full competition, the objective measurements help demonstrate the risk of re-injury when an athlete’s performance is compared to normal athletes in the same sport and age group.
A collision or a sudden change in direction may place unusually strong forces on the ligament and cause a partial or full tear.
SYMPTOMS
- Knee pain and difficulty walking
- Swollen knee (joint effusion)
- “Pop” may be heard or felt at the time of injury
Surgical reconstruction may be required. Surgery may involve reconstruction or the repair of other tissues inside the knee joint.
The round end of the femur (thigh bone) sits on the flat top of the tibia (shin bone) to make up the knee joint. The femur is supported by the meniscus, which is composed of two soft “c” shaped cartilage structures. These are soft, cushy cartilages that help the round thigh bone have a stable place on the shin bone. The one that sits on the inner side is called the medial meniscus, and the one on the outer side is called the lateral meniscus.
Three out of every 100 kids have an abnormally shaped lateral meniscus, and the condition is found more often in boys. Rather than having the typical “c” shape, the meniscus forms as a solid piece, similar to a Frisbee or disc. In addition to being shaped differently, the tissue also has an abnormal texture, which means it has a greater risk of causing problems. It is referred to as a discoid meniscus because of the disc shape.
A discoid meniscus does not always cause symptoms, and it may go unnoticed until symptoms begin. Alternatively, it may be discovered while another problem is being diagnosed in a child, adolescent or adult.
A discoid meniscus is not a condition that can be prevented. However, when symptoms present, proper diagnosis and management can reduce the risk of injuries that may cause long-term problems.
DIAGNOSIS
- A young child, age 4-7, can make his or her knee “pop” or “clunk” when they bend and straighten it. This doesn’t cause pain, and in most cases, does not need treatment.
- A preadolescent or adolescent athlete, age 9-17, has a forceful injury to the knee and tears ligaments. The meniscus looks torn, but it has often just folded or flipped over itself.
TREATMENT
In addition to changing the shape of the meniscus, a pediatric orthopedic specialist will evaluate the whole leg. The alignment of the hip, knee and ankle may put the discoid meniscus at further risk of damage as the child grows. As with many childhood orthopedic conditions, regular follow-up and monitoring of growth are important steps after a discoid meniscus is identified, even if treatment is not needed in the early stages.
A discoid meniscus should not prevent a young athlete from playing sports. When the decision to surgically change the shape of the meniscus is made, rehabilitation and a slow return to sports may be necessary.
Symptoms may include:
- Pain that worsens with activity
- Popping or clicking
- Swelling
X-rays are useful in diagnosing damage to the bone. Advanced imaging such as an MRI is helpful in evaluating damage to the cartilage and planning for surgery.
TREATMENT
Surgery may be needed when there are loose tissues in the joint, when the OCD appears to be getting worse on the imaging, when symptoms are getting worse (more fluid, catching or locking in the joint) or when OCD is diagnosed at later stages of the condition. With an arthroscope, pediatric orthopedic surgeons look inside the joint to better evaluate and manage the problem. Treatment may include reattaching or removing loose tissues, and in some cases, replacing lost tissue with new tissue.
After surgery, it may be a while before the athlete can return to running or contact sports. We recommend activities that keep children active, but are safe for the knee to allow healing. Swimming, diving, biking, golf and yoga are great examples.
Symptoms of a knee contusion depend on the severity of the injury and can include pain, swelling, discoloration/bruising, limping and inability to bear weight.
A thorough history and physical examination are used to diagnose a knee contusion. With significant swelling or discoloration, X-rays and/or advanced imaging, such as an ultrasound or MRI, may be ordered to rule out further damage.
For the first few days, manage swelling and discomfort as needed. Exercises can help improve strength and range of motion. Begin a home exercise program once the swelling has decreased and the pain has improved.
A knee contusion may cause discomfort for several weeks. However, after treatment, a full return to activity is expected.
- Proper fit of the patella in the groove on the femur
- Straight legs from hips to ankle (NOT knocked knees)
- Strong ligament attachments, including the medial patellofemoral ligament (MPFL)
Patellar instability is difficult to prevent since the anatomy of the leg bones cannot be changed easily. Some training for muscle strengthening and proper jumping and landing techniques may reduce the frequency of dislocations.
The history of the injury or injuries can often help a pediatric orthopedic provider properly diagnose this condition. X-rays and advanced imaging are important to confirm a diagnosis, evaluate leg alignment and identify other issues caused by the trauma of the dislocation.
Some patients have no complaints from their dislocations, or their chosen activities do not put the patella at risk of dislocating. Therefore, treatment for patellar instability is customized for the patient based on their history, activity level, chosen sport, age and other medical conditions.
After the first dislocation, the first step of treatment is to resolve any symptoms and swelling from the injury. Emergency care is recommended if the patella does not go back into place immediately. After symptoms have resolved, physical therapy and bracing are often recommended to identify any movement patterns or areas of weakness that make the patella function abnormally.
For some, patellar instability and dislocations can occur frequently. Surgical reconstruction of the MPFL is considered for patients who cannot perform basic daily skills or play sports.
Rehabilitation is an important component of recovery for a patient with patellar instability or dislocations. Learning to jump and land properly are important milestones in rehabilitation, especially for athletes returning to contact and stop-and-go sports. For those who have surgery, the progression of therapy is dependent on the recovery of the newly reconstructed ligament. Many athletes that have this procedure can return to competing in sports at their before-injury level.
The bone is at risk of injury in this area because it is a growth center. These soft tissue areas are considered open until the bone has completed growing here. Many growth centers have a ligament or tendon attached that can pull and, with repeated or significant force, can lead to an injury.
This problem is not very common and only occurs in growing children and adolescents. Because of that, it is best managed by pediatric specialists. Our team is leading a multi-center study to evaluate the treatment of this injury in order to identify quality standards and evidence-based treatment protocols across the nation.
Symptoms may include:
- Knee pain
- Swelling
- Knee stiffness
- Instability of the knee, often described as a feeling of giving way
Knowing the history of the injury or injuries can often help a pediatric orthopedic provider properly diagnose this condition. X-rays and advanced imaging are important to confirm a diagnosis and identify or rule out other issues caused by the injury.
If the fracture is stable, non-operative management with a cast or splint may be considered. Surgical intervention is typically an arthroscopic knee surgery that uses a screw to hold the bone fragment in place. A full evaluation of the knee to assess for other soft tissue damage is performed at the same time. In some cases, reconstruction of the ACL is necessary at the time of injury or may be required later because of the increased risk of injury to the ACL after a tibial spine fracture.
Many athletes return to sports after treatment for a tibial spine fracture. In some cases, stiffness in the knee joint may be a short-term concern, but it typically does not cause any long-term consequences.
Osgood-Schlatter disease commonly occurs in children between 9 and 15 years of age. Typically, symptoms are worse during a period of rapid growth and increased activity. Children participating in certain activities, including soccer, gymnastics, basketball and distance running, are more susceptible to this problem. It is also more common in boys than it is in girls.
Symptoms typically include
- Knee pain with activity like running, jumping or going up and down stairs
- Swelling or a bump below the knee cap (on the tibial tubercle)
- Tenderness below the knee cap
- Limping that may get worse after activity
Osgood-Schlatter disease may be difficult to prevent. Proper warm-up and stretching exercises of the upper leg and lower leg muscles may help. Your child should avoid overtraining by limiting activity when pain is present.
This condition can be diagnosed with a thorough history and physical exam. In some cases, X-rays may be ordered to rule out other issues.
Treatment
- Manage pain and swelling
- Rest from activities that cause pain
- A knee strap or neoprene knee sleeve may assist with improving soreness
- Exercises focused on flexibility of the leg muscles, including the quadriceps and the hamstrings
The patellofemoral joint is located in the front of the knee, where the kneecap and femur (thigh bone) come together. This joint can become inflamed and cause pain in children and adolescents.
The most common cause is overuse, or repetitive and prolonged activities that involve bending and straightening of the knee.
Other factors that can cause or make the condition worse include:
- Impact activities, such as running, jumping, squatting and using stairs
- Weakness and/or poor flexibility of the hip, leg, and core muscles
- Improper form during movement, sport or exercise
- Abnormal alignment of the lower body or kneecap
- Running on hard or uneven surfaces
- Falling on the kneecap or other direct impacts to the area
- Exercising too much in a short period of time or increasing activity too quickly
- Rapid growth in height
- Pain under, around or behind the kneecap, often in a “U” shaped pattern
- Pain that often gets worse during or after these activities:
- Walking or running
- Repetitive jumping
- Sitting for a long time
- Walking downhill
- Walking up or down stairs
- A grinding sensation under the kneecap
- Vary training to allow rest and avoid overuse from repetitive activities
- Do proper stretching exercises before and after activities
- Avoid excessive training by limiting activity that causes pain and stop activities if pain returns
- Wear proper fitting shoes
Treatment is focused on providing comfort and improving the alignment of the joint during activities, and may include:
- A home exercise program or physical therapy program. Goals include:
- Stretching and strengthening hip, core, thigh and leg muscles
- Learning proper form for movements, including stair climbing, running, squats and sport-specific movements, such as jumping and landing
- A knee support device, such as a brace, sleeve or strap to help with soreness or pain
- Supportive and properly fitted shoes
- Shoe inserts for over-pronation (movement that flattens the foot) if recommended by your provider
The patellar tendon attaches the apophysis (a growth plate) of the patella (kneecap) to the shinbone. This area is made up of soft cells called cartilage. These weaker cells are at a higher risk of injury. Repeated pulling of the patellar tendon on the apophysis causes inflammation and irritation. This commonly occurs during periods of rapid growth or increased activity.
Additional factors that may contribute to SLJ syndrome:
- Playing sports, like basketball, that involve running and jumping
- Going up and down stairs
- Playing only one sport, overuse or overtraining
Symptoms may include:
- Tenderness or pain near the bottom of the kneecap
- Swelling or inflammation around the kneecap
- Knee pain or limping with activities like running, jumping, kneeling or going up and down stairs
- Pain following a direct impact to the knee
A thorough history and physical examination are used to diagnose SLJ syndrome. In some cases, X-rays may be ordered to rule out other issues.
Treatment includes avoiding activities that hurt and managing discomfort as needed.
- Limit or change the activities that cause symptoms
- Wear a knee strap or neoprene knee sleeve to help reduce tension around the tendon, soreness or pain
- Stretch the leg muscles, including the quadriceps and the hamstrings, to help reduce tension on the tendon

Bridge Program and Training Classes
Young athletes cleared from therapy but not quite ready to get back to sport should check out our Bridge Program. Get ready to return safely to sports with our team of strength and conditioning coaches in Frisco. Additionally, our coaches offer a variety of performance courses to help improve muscle strength and movement quality and help prevent future injuries.
Learn more here: What is the Bridge Program?