Oct 26, 2018 / Sports Medicine
A Leader Among Us
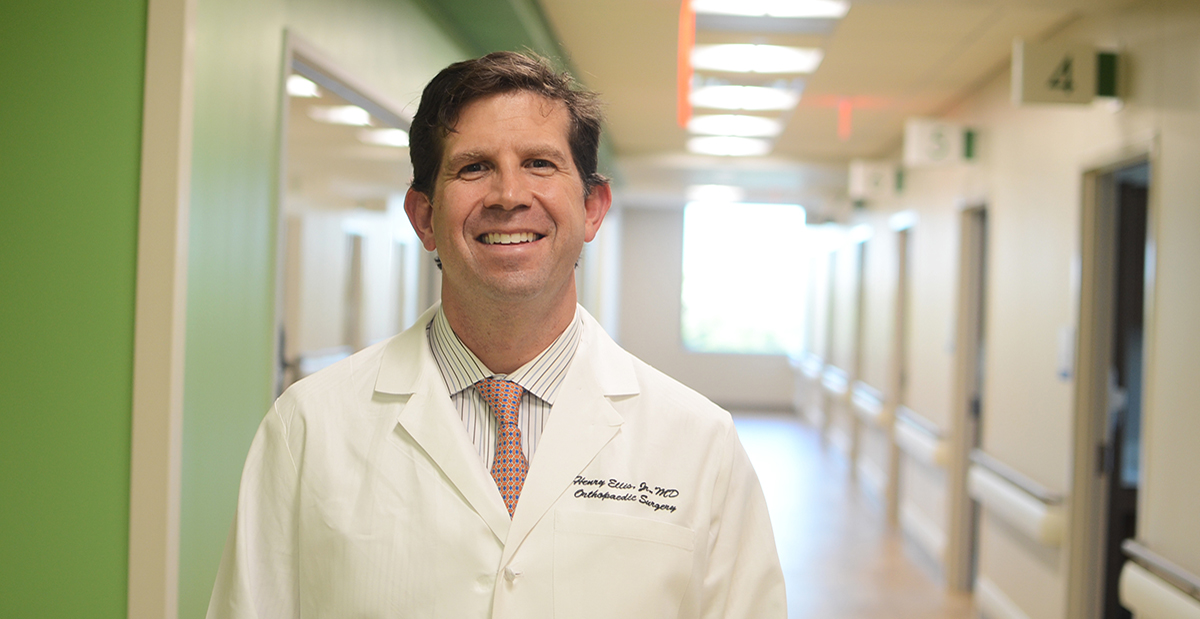
As a member of the American Academy of Orthopaedic Surgeons Leadership Fellows Program and member of the Texas Orthopaedic Association’s Leadership Council, Henry B. Ellis, M.D., Scottish Rite Hospital pediatric orthopedic surgeon was recently interviewed by the Texas Orthopedic Association.
The interview covers his thoughts on his role in advocacy, our new campus in Frisco and his thoughts on the future of orthopedic.
TOA: Many tend to think of the Texas Scottish Rite Hospital for Children (TSR) as an institution that focuses on scoliosis and other less common orthopaedic conditions. How did you decide to take your sports medicine focus to TSR and its Frisco campus?
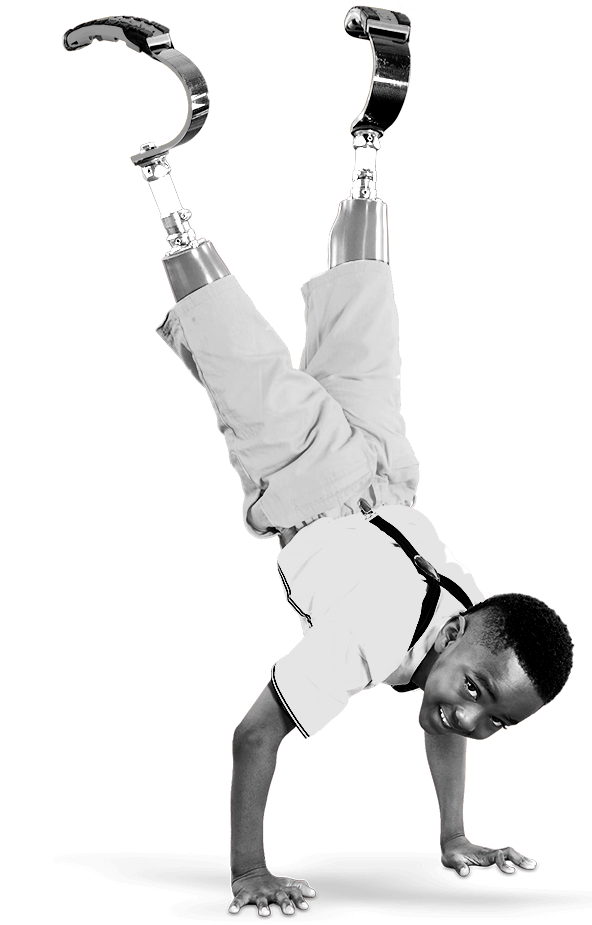
Ellis: TSR has a long legacy of addressing the North Texas community by being a resource for kids with the greatest need. In the early years, one of the hospital’s primary mission was in the treatment of polio in children. Since the eradication of polio, we have focused on other orthopedic problems in kids, such as scoliosis, clubfoot, and hip dysplasia, to name a few.
Now that sports injuries and overuse are such large epidemics in youth musculoskeletal care, Frisco is the right place to continue the mission of care of these kids. Our main and primary focus is on the skeletally immature athletes and we hope to continue the hospital’s legacy and mission to treat the pediatric patient with the greatest need in our community.
The overwhelming popularity of youth sports that has subsequently evolved to have a resultant increase in pediatric sports-related acute and overuse injuries. Secondly, newer surgical techniques have been developed and popularized, such as an extra-physeal ACL reconstruction, that have improved our ability to treat young athletes with severe injuries and with open growth plates.
TOA: What is the timeline for TSR’s new facility in Frisco?
Ellis: Our first patient at the new Frisco campus is on October 10, with the ambulatory surgery center opening shortly thereafter. Our pediatric physical therapy and sport therapy service with a motion science lab will also begin to treat patients on October 10. All pediatric orthopaedic specialty clinics will also begin on October 10.
TOA: You have become more engaged in orthopaedic leadership over the past few years through the AAOS leadership, TOA’s Leadership Council, and visits with both TOA and AAOS to Washington, DC. What has surprised you about being engaged in orthopaedic leadership?
Ellis: The biggest surprise to me has been the value of advocacy and how is relates to my practice and the hospital. My initial impression was there was little role for an orthopaedic surgeon or its organization to significantly influence more than just reimbursements. But I have witnessed how TOA and AAOS plays a role in regulatory reform, opioid management, team physician protection, and on and on. It has now become clear to me that there is an important value of a collaborative effort to protect our specialty.
TOA: What do you tell residents about how to prepare for their future practice?
Ellis: Once residents begin to get comfortable with the basic of orthopaedic surgery and the musculoskeletal system, they need to start opening their eyes and ears to the “how” to build a successful practice. I learned most of my tricks in billing, not from a course, but from constantly asking mentors how they coded or billed for something or the finances behind their practice (ie overhead cost).
Secondly, no one in residency specifically teaches the importance of securing referral patterns. There is an old saying (also referred to as the three “A’s” of medicine) that one must be available, affable, and able. This includes all phones calls, texts, or emails from referring providers no matter how frustrating or inconvenient it is at the time. Too often in residency we got over burdened with calls for, what we thought, were insignificant consults. When starting a practice, these “insignificant consults” become valuable and you will transition your response to be more welcoming to develop a relationship with the referring provider.
TOA: You have many years of practice ahead of you in the Dallas-Fort Worth area. Looking into your crystal ball, what do you see for the future of orthopaedics in Texas?
Ellis: Tough question. Telemedicine will certainly be an invaluable and integral part of an orthopaedic surgeon’s practice, and especially in Texas with the large rural countryside and underserved areas. During our recent trip to DC, Congressman Beto O’Rourke asked us (TOA) how we could recruit quality orthopaedic surgeons to rural Texas. As we know the answer may be complex, however, telemedicine would certainly allow for a provisional discussion with a patient, video examination, and radiographic review. Telemedicine will be in the future of orthopaedics in Texas and not only for rural Texas, but for urban urgent care consultation or for a follow up assessment. There is no substitute for a live history and physical for definitive treatment recommendations, but we make many of our decision today largely based on the x-ray and MRI. I have used a limited version of telemedicine and have found value, convenience, and patient satisfaction with its use.
For information about injury prevention and pediatric sports medicine, please visit our website at scottishritehospital.org/sports.
The interview covers his thoughts on his role in advocacy, our new campus in Frisco and his thoughts on the future of orthopedic.
TOA: Many tend to think of the Texas Scottish Rite Hospital for Children (TSR) as an institution that focuses on scoliosis and other less common orthopaedic conditions. How did you decide to take your sports medicine focus to TSR and its Frisco campus?
Ellis: TSR has a long legacy of addressing the North Texas community by being a resource for kids with the greatest need. In the early years, one of the hospital’s primary mission was in the treatment of polio in children. Since the eradication of polio, we have focused on other orthopedic problems in kids, such as scoliosis, clubfoot, and hip dysplasia, to name a few.
Now that sports injuries and overuse are such large epidemics in youth musculoskeletal care, Frisco is the right place to continue the mission of care of these kids. Our main and primary focus is on the skeletally immature athletes and we hope to continue the hospital’s legacy and mission to treat the pediatric patient with the greatest need in our community.
The overwhelming popularity of youth sports that has subsequently evolved to have a resultant increase in pediatric sports-related acute and overuse injuries. Secondly, newer surgical techniques have been developed and popularized, such as an extra-physeal ACL reconstruction, that have improved our ability to treat young athletes with severe injuries and with open growth plates.
TOA: What is the timeline for TSR’s new facility in Frisco?
Ellis: Our first patient at the new Frisco campus is on October 10, with the ambulatory surgery center opening shortly thereafter. Our pediatric physical therapy and sport therapy service with a motion science lab will also begin to treat patients on October 10. All pediatric orthopaedic specialty clinics will also begin on October 10.
TOA: You have become more engaged in orthopaedic leadership over the past few years through the AAOS leadership, TOA’s Leadership Council, and visits with both TOA and AAOS to Washington, DC. What has surprised you about being engaged in orthopaedic leadership?
Ellis: The biggest surprise to me has been the value of advocacy and how is relates to my practice and the hospital. My initial impression was there was little role for an orthopaedic surgeon or its organization to significantly influence more than just reimbursements. But I have witnessed how TOA and AAOS plays a role in regulatory reform, opioid management, team physician protection, and on and on. It has now become clear to me that there is an important value of a collaborative effort to protect our specialty.
TOA: What do you tell residents about how to prepare for their future practice?
Ellis: Once residents begin to get comfortable with the basic of orthopaedic surgery and the musculoskeletal system, they need to start opening their eyes and ears to the “how” to build a successful practice. I learned most of my tricks in billing, not from a course, but from constantly asking mentors how they coded or billed for something or the finances behind their practice (ie overhead cost).
Secondly, no one in residency specifically teaches the importance of securing referral patterns. There is an old saying (also referred to as the three “A’s” of medicine) that one must be available, affable, and able. This includes all phones calls, texts, or emails from referring providers no matter how frustrating or inconvenient it is at the time. Too often in residency we got over burdened with calls for, what we thought, were insignificant consults. When starting a practice, these “insignificant consults” become valuable and you will transition your response to be more welcoming to develop a relationship with the referring provider.
TOA: You have many years of practice ahead of you in the Dallas-Fort Worth area. Looking into your crystal ball, what do you see for the future of orthopaedics in Texas?
Ellis: Tough question. Telemedicine will certainly be an invaluable and integral part of an orthopaedic surgeon’s practice, and especially in Texas with the large rural countryside and underserved areas. During our recent trip to DC, Congressman Beto O’Rourke asked us (TOA) how we could recruit quality orthopaedic surgeons to rural Texas. As we know the answer may be complex, however, telemedicine would certainly allow for a provisional discussion with a patient, video examination, and radiographic review. Telemedicine will be in the future of orthopaedics in Texas and not only for rural Texas, but for urban urgent care consultation or for a follow up assessment. There is no substitute for a live history and physical for definitive treatment recommendations, but we make many of our decision today largely based on the x-ray and MRI. I have used a limited version of telemedicine and have found value, convenience, and patient satisfaction with its use.
For information about injury prevention and pediatric sports medicine, please visit our website at scottishritehospital.org/sports.