Jun 15, 2020 / Sports Medicine
Evaluation and Management of Sport-Related Concussions
The following is a summary of a presentation on sport-related concussions in young athletes by Shane M. Miller, M.D., pediatric sports medicine physician. The lecture was given as part of the Coffee, Kids and Sports Medicine series and is available in our on-demand learning offerings.
Watch the full lecture I Print the PDF
A concussion is a brain injury.
There are many misunderstandings that persist despite growing concern and awareness of sport-related concussions. The lecture covers these and more.
Children and adolescents may not report or even recognize all concussion-related symptoms. Therefore, using a standardize symptom scale (i.e., Post-Concussion Symptom Scale, Sport Concussion Assessment Tool 5 (pediatric version for < 12 years), Graded Symptom Checklist) is necessary to ensure assessment across several categories including:
A thorough evaluation is time-consuming but necessary to assess for all potential impairments. The concussion evaluation includes:
Partnering with school athletic trainers, nurses and administrators can smooth the athlete’s transition back to schoolwork. The clinical report in Pediatrics (2013) provides a template for return to learn recommendations in a checklist format.
Return to Activity
It is common for teenagers to have symptoms for several weeks, but most will fully recover in less than four weeks. Restricting physical activity for this long has been shown to be detrimental. Symptom-limited, light aerobic exercise after at most 2-3 days of rest is believed to be safe and beneficial.
Return to Sport
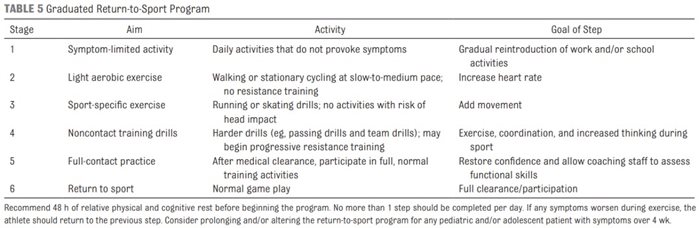
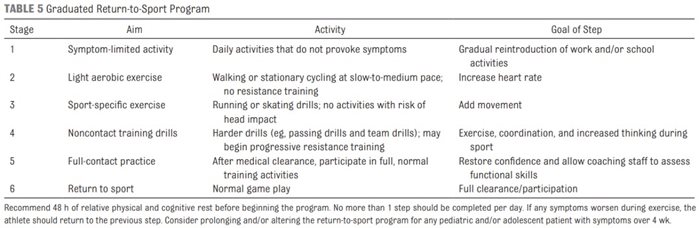
In Texas, athletes in University Interscholastic League (UIL) Sports are required to have a physician (M.D. or D.O.) clearance for return to play. The process must occur gradually and must not cause symptoms to return. Below is an example of a gradual return to sport progression.
Prolonged Recovery
With continued progress in concussion research, there is an improved understanding of who may experience a prolonged recovery. These include, but are not limited to:
Partnering with specialists can improve outcomes for young athletes but is not always necessary. Our team is multidisciplinary and concussion treatment may include interventions by physical therapists, neurologists, psychologists, athletic trainers, etc. Miller specifically suggests that patients with prolonged recovery (> one month), worsening symptoms, or those with a history of multiple concussions and difficulty with making return to play decisions, will benefit from specialist consultation.
Scottish Rite for Children conducts and is actively involved in multi-center local and national research studies to evaluate concussions throughout the course of recovery and well-beyond return to play. Inviting patients to participate in these studies in the acute stage is particularly helpful as we further evolve the understanding of concussion recognition, treatment, management and return to play decision making for all.
Resources for Further Review
Below are the primary sources for guidance on concussion recognition, management and return to play. Miller, with a sound understanding of these and extensive experience managing thousands of young athletes, highlights the key messages in these resources that apply to pediatric and adolescent patients.
CDC Guidelines emphasize the following:
Watch the full lecture I Print the PDF
A concussion is a brain injury.
There are many misunderstandings that persist despite growing concern and awareness of sport-related concussions. The lecture covers these and more.
- A concussion is caused by a direct blow OR “impulsive” force transmitted to the head. An athlete does not require direct head contact with the ground or another athlete to sustain a concussion.
- A concussion is an impairment of neurological function. There are no abnormalities noted on standard neuroimaging studies used in clinical practice (CT or MRI). Do not routinely image pediatric patients. Use a clinical decision tool (i.e. PECARN criteria) for imaging.
- The majority of athletes do not lose consciousness with a concussion.
- Grading concussions is no longer recommended. The severity of the impairments is often not fully understood until the athlete has recovered, and it is difficult to predict recovery times.
- Most concussions do not need to be evaluated in the emergency room. Learning the “red flags” to know when an urgent evaluation is warranted for existing or worsening symptoms.
- LATEST recommendations for treatment are to modify activity levels based on the individual athlete’s symptoms as they return to school, activities and sports. Strict rest and restriction from electronic devices are not necessary. Prolonged absences from school and physical activity restrictions may prolong recovery.
Children and adolescents may not report or even recognize all concussion-related symptoms. Therefore, using a standardize symptom scale (i.e., Post-Concussion Symptom Scale, Sport Concussion Assessment Tool 5 (pediatric version for < 12 years), Graded Symptom Checklist) is necessary to ensure assessment across several categories including:
- Cognitive
- Physical
- Emotional/Mood
- Sleep Disturbance
A thorough evaluation is time-consuming but necessary to assess for all potential impairments. The concussion evaluation includes:
- Physical exam
- Neurological exam
- Balance assessment
- Vestibular-ocular motor screen (VOMS)
- Neurocognitive testing
- with poor balance may be at higher risk of new or repeat concussion or musculoskeletal injuries if returning to sport too soon.
- with positive findings on VOMS testing, they may experience symptom worsening while doing schoolwork that requires scanning or alternating focus from teacher to desk.
- that reports no symptoms, but performs these physical exams poorly, may not be under reporting symptoms in order to return to sports prior to complete recovery.
Partnering with school athletic trainers, nurses and administrators can smooth the athlete’s transition back to schoolwork. The clinical report in Pediatrics (2013) provides a template for return to learn recommendations in a checklist format.
Return to Activity
It is common for teenagers to have symptoms for several weeks, but most will fully recover in less than four weeks. Restricting physical activity for this long has been shown to be detrimental. Symptom-limited, light aerobic exercise after at most 2-3 days of rest is believed to be safe and beneficial.
Return to Sport
In Texas, athletes in University Interscholastic League (UIL) Sports are required to have a physician (M.D. or D.O.) clearance for return to play. The process must occur gradually and must not cause symptoms to return. Below is an example of a gradual return to sport progression.
Prolonged Recovery
With continued progress in concussion research, there is an improved understanding of who may experience a prolonged recovery. These include, but are not limited to:
- previous history of mTBI
- neurological or psychological disorder
- learning difficulties
- older children/adolescents
- lower socioeconomic status
- female sex
- greater number or severity of symptoms
Partnering with specialists can improve outcomes for young athletes but is not always necessary. Our team is multidisciplinary and concussion treatment may include interventions by physical therapists, neurologists, psychologists, athletic trainers, etc. Miller specifically suggests that patients with prolonged recovery (> one month), worsening symptoms, or those with a history of multiple concussions and difficulty with making return to play decisions, will benefit from specialist consultation.
Scottish Rite for Children conducts and is actively involved in multi-center local and national research studies to evaluate concussions throughout the course of recovery and well-beyond return to play. Inviting patients to participate in these studies in the acute stage is particularly helpful as we further evolve the understanding of concussion recognition, treatment, management and return to play decision making for all.
Resources for Further Review
Below are the primary sources for guidance on concussion recognition, management and return to play. Miller, with a sound understanding of these and extensive experience managing thousands of young athletes, highlights the key messages in these resources that apply to pediatric and adolescent patients.
- Consensus statement on concussion in sport – the 5th international conference on concussion in sport (most recent Berlin, 2016, next in Paris, 2021)
- Center for Disease Control and Prevention Guideline on the Diagnosis and Management of Mild Traumatic Brain Injury Among Children
- American Academy of Pediatrics (AAP) Sport-Related Concussion in Children and Adolescents – update on position statement published in Pediatrics (2013)
- American Medical Society for Sports Medicine (AMSSM) position statement – includes a new visual approach to describe clinical profiles that may help to better target recommendations and interventions
- Texas House Bill (HB) 2038 – Texas law established in 2011, all fifty states had a similar law established between 2009 and 2014; almost all include education, return to play and medical clearance
CDC Guidelines emphasize the following:
- Do not routinely image patients to diagnose mTBI.
- Use validated, age-appropriate symptom scales to diagnose mTBI.
- Assess evidence-based risk factors for prolonged recovery.
- Provide patients with instructions on return to activity customized to their symptoms.
- Counsel patients to return gradually to non-sports activities after no more than 2-3 days of rest.